Image: Midjourney/ MomJunction Design Team
Athlete’s foot in children is a fungal infection, which usually affects the skin of the feet, especially between the toes. The primary sign of the infection is the reddish-white appearance of the skin. The affected area may also become itchy, moist, and scaly. It is called an athlete’s foot since it is most commonly observed among athletes.

Children may risk catching this fungal infection if they frequently use public showers, swimming pools, or locker rooms without footwear. Although the infection usually resolves with topical antifungal medications, parents must recognize its signs and seek medical advice to treat it effectively and prevent repeated infections. This post tells you more about athlete’s foot in children, its symptoms, and how to prevent it.
Key Pointers
- Athlete’s foot is a fungal infection caused by dermatophytes.
- Walking barefoot on dirty floors or wearing shoes that do not have proper ventilation increases the risk of infections.
- Infected skin cracks and cheese-like skin between toes are common signs of Athlete’s foot.
- Washing feet often, wearing clean cotton socks, and other preventive measures as you scroll through.
What Causes Athlete’s Foot In Children?
Athlete’s foot, also known as tinea pedis or foot ringwormiA skin infection caused by fungus resulting in red circular rashes. , is caused by a fungus belonging to the dermatophytesiA group of fungi responsible for ringworm infection. group of fungi (1). The groups of fungi associated with this are trichophyton rubrum, epidermophyton floccosumi A type of filamentous fungus which causes skin and nail infections , trichophyton tonsurans, and trichophyton mentagrophytes (2) (24). The infections caused by these fungi are known as tinea infections. These fungi thrive in humid and warm conditions and are predominant in damp places full of moisture, such as showers, swimming pools, and locker rooms. Their fungal spores can survive for a long time in favorable conditions and spread the infection (2).
According to the St. Louis Children’s Hospital, this fungal infection is less likely to affect children before puberty (3). It mostly affects teens and young adults (4). However, there are also reports of a rare incidence of tinea pedis in two to four percent of school-aged children (25).
 Quick Tip
Quick TipRisk Factors For Athlete’s Foot

The following conditions and situations increase a child’s risk of developing athlete’s foot (5) (6).
- Walking barefoot on contaminated floors, like those in locker rooms or public showers where the contagious fungus may thrive.
- Wearing shoes that do not provide the feet with adequate ventilation.
- Keeping the feet wet for a long time after a shower or swim.
- Sweating profusely due to exercise or hyperhidrosis (excessive sweating).
- Sharing socks, towels, or shoes with others.
Signs and Symptoms Of Athlete’s Foot In Children
Children with athlete’s foot show the following signs.
- Infected skin cracks and blisters that cause discomfort
- Peeling skin between the toes
- Redness, and formation of scales on the soles of the feet
- Reddish-white patches or blisters between the toes that cause terrible itching
- Sting- or burn-like sensation felt in the affected skin
- Cheese-like skin between the toes, with a foul odor
- Itchy blisters may appear soggy and ooze fluid.
The athlete’s foot can spread to other body parts through contact.
When the infection spreads to the groin area and armpits, then it is known as jock itch. Generally, Jock itch (Tinea Cruris) in kids is harmless and can be effectively treated using over-the-counter antifungal creams or ointments.
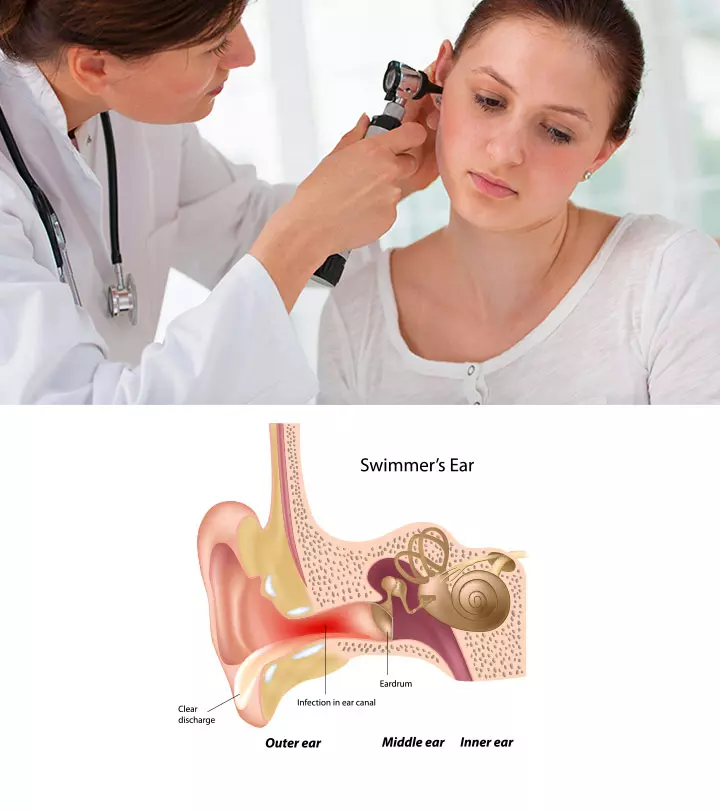
Diagnosis And Treatment For Athlete’s Foot

The healthcare provider can diagnose the condition through visual inspection of the affected skin.
- They may ask about the child’s medical history and enquire about the use of public sports facilities, swimming pools, or showers.
- If a visual inspection is not sufficient, the doctor may examine skin scrapings under the microscope to determine the presence of fungus.
- Athlete’s foot can be treated with topical antifungal creams or powders. Pediatrician Dr. Raashid Hamid says, “Antifungal powders can help effectively manage an athlete’s foot, especially for active kids who sweat a lot. Applying antifungal powder to the feet and inside shoes can help soak moisture and create an inhospitable environment for fungi.”
- Creams containing miconazole, clotrimazole, terbinafine, or butenafine may be prescribed by a doctor (24).
- Your child may have to use the cream for a week or two after the infection is cleared, to prevent recurrence (7).
- Oral antifungal medications such as fluconazole or terbinafine may be prescribed in severe cases (24).
- If the child is getting a recurrent infection, the doctor might advise a blood test for diabetes.
 Quick Tip
Quick TipWhat Is the Best OTC Medicine For An Athlete’s Foot?
Medications containing active ingredients like Terbinafine and Clotrimazole are commonly recommended to treat athlete’s foot. The most frequently used products typically contain allylamines or azoles, which work by inhibiting or killing the growth of the fungus (8). These antifungal drugs are available without a prescription in various forms such as creams, gels, and sprays. Consult with your child’s doctor to learn the right product and formulation that works best for them.
Home Remedies For Athlete’s Foot
Home remedies may help relieve the symptoms of athlete’s foot. Do note that these remedies have limited scientific evidence. Let your child’s doctor know before using these remedies to prevent interference with the treatment.
1. Tea tree oil

According to a study, tea tree oil is said to have antifungal activity against dermatophytes (9). Regular application of tea tree oil is said to reduce the symptoms of athlete’s foot.
Mix tea tree oil in coconut oil in the proportion of 1:2 and apply it on the affected area. Repeat this twice daily.
2. Garlic
Garlic’s antifungal properties make it a topical antifungal agent (10). Crush a few garlic cloves and rub them on the affected area and rinse it after 15 minutes. Repeat these steps twice daily.
3. Neem
Neem is proven to be effective against dermatophytes. You can apply neem oil or neem leaves paste on the affected area. Repeat it twice or thrice a day (11).
4. Sea salt

Sea salt is also known for its antifungal property (12). Mix a cup of sea salt in a small tub of warm water and let your child soak their feet for at least 20 minutes. However, do remember to dry their feet thoroughly post soaking.
5. Talcum powder
Anecdotal evidence suggests that talcum or baby powder might help relieve the athlete’s foot symptoms by keeping the affected area clean and dry.
Apply talcum powder all over your child’s feet before putting on the socks. Repeat this every time they wear shoes.
6. Baking soda
Studies found that baking soda was able to inhibit the growth of dermatophytes. It could be used as a topical antifungal agent to relieve the symptoms of athlete’s foot (13).
Make a paste by mixing baking soda in water, apply it on the affected area, and let it remain for 15 minutes. Rinse and repeat twice daily.
 Quick Tip
Quick TipPrevention Of Athlete’s Foot In Children

Board-certified diplomate of the Philippine Pediatric Society, Dr. Maria Carmela Villania-Mamauag, advises, “Athlete’s foot, in general, is a fungal infection caused by improper hygiene and exposure to unsanitary conditions. Hence, observance of good hygiene practices (daily baths, keeping the feet dry, clipping the nails regularly, etc.) and appropriate and clean footwear are basic steps in avoiding having athlete’s foot.”
Here are some simple lifestyle changes and precautions to prevent athlete’s foot (14) (15):
- Make it a habit for your child to wash their feet and dry them thoroughly after walking barefoot outdoors.
- Ensure your child dries their feet (especially the area between the toes) after taking a shower.
- Make your child wear shower shoes in public showers to prevent their feet from touching the floor.
- Choose breathable shoes and avoid tight-fitting footwear that lock moisture.
- Provide them with clean cotton socks.
- Change your child’s socks daily and wash them with a disinfectant.
- Never let your child share towels, shoes, or clothes with others.
- Clip nails periodically since fungal spores can lodge themselves under the nails.
- Sun-dry washed shoes thoroughly before using them again.
Possible Complications Of Athlete’s Foot In Children
Athlete’s foot is a mild and common skin infection that cures with treatment within weeks
. In rare instances, a delay in the treatment may cause the following complications (16).
- Impetigo: Athlete’s foot can cause the skin to crack open, thus permitting the entry of bacteria. It could lead to impetigo, a superficial bacterial infection of the skin.
- Cellulitis: If bacteria spread to the deeper layers of the skin, fat, and soft tissues, then they cause cellulitis. It is characterized by red patches that are hot and tender to touch.
- Onychomycosis: The fungus from the skin of the feet can spread to the toenails to cause onychomycosis. This fungal nail infection in children tends to run in families; however, not everyone is susceptible.
 Quick Tip
Quick TipBacterial infections require antibiotic treatment. Fungal nail infection may require additional medications like oral antifungals for a long duration.
Frequently Asked Questions
1. What can be mistaken for an athlete’s foot?
EczemaiA medical condition in which skin develops rough patches with blisters. , dry skin, psoriasisiA skin condition characterized by rough, itchy, and flaky patches predominantly seen on knees, elbows, or scalp. , and pityriasis roseaiA skin infection that starts with oval-shaped rashes on the face, chest, abdomen, or back. are a few conditions that may be mistaken for athlete’s foot (17) (18).
2. Can an athlete’s foot in children go away on its own?
Athlete’s foot is unlikely to self-resolve and usually will require anti-fungal medication, including over-the-counter topical creams for relief (19).
3. What are the differences between an athlete’s foot in adults and children?
There are no known differences in the symptoms of an athlete’s foot in children and adults. However, although the fundamental features and treatment of an athlete’s foot are comparable in both age groups, it’s essential to recognize that individual instances may differ. Therefore, it is advisable to consult a healthcare professional for precise diagnosis, suitable treatment choices, and personalized care, particularly for pediatric cases.
4. What are the common misconceptions about athlete’s foot in children?
One common misconception regarding an athlete’s foot is that it is non-contagious. On the contrary, it is a highly contagious type of ringworm in kids that easily spreads in areas such as locker rooms or showers and can be transmitted through minor skin cuts on foot (20).
5. What causes a recurring athlete’s foot?
Recurrent infections may result from fungi that linger on footwear (socks or shoes).
Additionally, warm and humid conditions, poor foot hygiene, and walking barefoot in public places can increase the risk. To prevent recurrence, it’s crucial to undergo thorough treatment, follow proper foot hygiene, and avoid potentially contaminated areas. If the problem persists, seek advice from a medical professional (19).
6. Is turmeric powder good for an athlete’s foot?
Dr. Christina Johns, a Maryland-based pediatrician, says, “Turmeric has anti-inflammatory and antifungal characteristics and is utilized by some as a natural treatment for various skin issues. Having said that, there is limited scientific proof to back the use of turmeric specifically for athletes’ foot, and its efficiency might differ among individuals.”
Accumulation of sweat or wetness from walking barefoot may lead to fungal growth between toes causing Athlete’s foot or tinea pedis. It is treatable with antifungal medication. However, it is better to check with your doctor before using any ointment or cream or home remedies such as tea tree oil, garlic, neem, or baking soda. Untreated Athlete’s feet in children may cause bacterial infections due to deep cracks or toenail fungal infections. Ensure your child follows basic foot hygiene to keep the toes clean and dry to prevent fungus from growing.
Infographic: Treatments And Care Advice For Athlete’s Foot In Children
Athlete’s foot in children can be cured with adequate foot care and medications. If left untreated, it may spread to nails and other parts of the skin. Go through the infographic to know the common treatments and ways to care for an athlete’s foot in children.
Some thing wrong with infographic shortcode. please verify shortcode syntax
Discover effective methods to address athlete’s foot. Obtain valuable insights on preventing and managing this prevalent condition with expert tips and guidance.
References
- Tinea (Ringworm Jock Itch Athlete’s Foot); John Hopkins Medicine
https://www.hopkinsmedicine.org/all-childrens-hospital/patient-families - Nkatoko Freddy Makola et al. Managing athlete’s foot; South African Family Practice
https://www.ajol.info/index.php/safp/article/download/183760/173117 - Athlete’s Foot; St. Louis Children’s Hospital
https://www.stlouischildrens.org/conditions-treatments/athletes-foot - Tinea pedis; DermNet NZ
https://dermnetnz.org/topics/tinea-pedis - Athlete’s foot; U.S. National Library of Medicine
https://medlineplus.gov/ency/article/000875.htm - Athlete’s Foot; University of Michigan
https://www.uofmhealth.org/health-library/hw28392 - What is Athlete’s Foot?; Penn Medicine
https://www.pennmedicine.org/for-patients-and-visitors/patient-information/conditions-treated-a-to-z/athletes-foot - What helps to get rid of athlete’s foot?; National Library of Medicine
https://www.ncbi.nlm.nih.gov/books/NBK279548/ - Andrew C Satchell et al. Treatment of interdigital tinea pedis with 25% and 50% tea tree oil solution: a randomized placebo-controlled blinded study
https://www.google.com/url?q=https://pubmed.ncbi.nlm.nih.gov/12121393/&sa=D&source=docs&ust=1701078069798170&usg=AOvVaw3-ps5oQwO25vFhvhNcd0g6 - Farzad Aala et al. Inhibitory effect of allicin and garlic extracts on growth of cultured hyphae; NCBI
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4016684/ - Neem: A Tree For Solving Global Problems; NCBI
https://www.ncbi.nlm.nih.gov/books/NBK234637/ - Michelle Pirrie Stockwell John Clulow and Michael Joseph Mahony; Sodium Chloride Inhibits the Growth and Infective Capacity of the Amphibian Chytrid Fungus and Increases Host Survival Rates; NCBI
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3349647/ - V Letscher-Bru et al. Antifungal activity of sodium bicarbonate against fungal agents causing superficial infections; NIH
https://pubmed.ncbi.nlm.nih.gov/22991095/ - How to Prevent Athlete’s Foot.
https://www.aad.org/public/diseases/a-z/athletes-foot-prevent - Athlete’s foot | Tinea pedis U.S. National Library of Medicine
https://medlineplus.gov/athletesfoot.html - Athlete’s foot; Health Service Executive
https://www2.hse.ie/conditions - Ask the doctor: Athlete’s foot that won’t quit; Harvard Health Publishing
https://www.health.harvard.edu/diseases-and-conditions/ask-the-doctor-athletes-foot-that-wont-quit - Tinea Infection; University of Rochester
https://www.urmc.rochester.edu/encyclopedia/content.aspx?contenttypeid=85&contentid=P00310 - Athlete’s foot; NHS
https://www.nhs.uk/conditions/athletes-foot/#:~:text=Athlete’s%20foot%20is%20unlikely%20to - Ten ‘feet treats’ that do more harm than good; Temple Now
https://news.temple.edu/news/ten-%E2%80%98feet-treats%E2%80%99-do-more-harm-good - Nigam PK, Syed HA, Saleh D.; Tinea Pedis; National Library of Medicine
https://www.ncbi.nlm.nih.gov/books/NBK470421/ - Athlete’s Foot; Seattle Children’s Hospital
https://www.seattlechildrens.org/conditions/a-z/athletes-foot/ - CARD9 Deficiency; National Organization for Rare Disorders
https://rarediseases.org/rare-diseases/card9-deficiency/ - Common Tinea Infections in Children; American Academy of Family Physicians.
https://www.aafp.org/pubs/afp/issues/2008/0515/p1415.html#:~:text=Topical%20antifungal%20agents,or%20refractory%20infections. - Sheila Fallon Friedlander; Tinea Pedis (Athlete’s Foot), Principles and Practice of Pediatric Infectious Diseases.
https://www.sciencedirect.com/topics/pharmacology-toxicology-and-pharmaceutical-science/tinea-pedis
Community Experiences
Join the conversation and become a part of our nurturing community! Share your stories, experiences, and insights to connect with fellow parents.
Read full bio of Dr. Anuradha Bansal
- Dr. Raashid Hamid is a consultant in the department of Pediatric Surgery at GMC hospital and associate professor of Pediatric and Neonatal Surgery at SKIMS, Jammu & Kashmir, India. He has four years of experience and specializes in general surgeries, including appendectomy, cholecystectomy, and exploratory laparotomy.
 Dr. Raashid Hamid is a consultant in the department of Pediatric Surgery at GMC hospital and associate professor of Pediatric and Neonatal Surgery at SKIMS, Jammu & Kashmir, India. He has four years of experience and specializes in general surgeries, including appendectomy, cholecystectomy, and exploratory laparotomy.
Dr. Raashid Hamid is a consultant in the department of Pediatric Surgery at GMC hospital and associate professor of Pediatric and Neonatal Surgery at SKIMS, Jammu & Kashmir, India. He has four years of experience and specializes in general surgeries, including appendectomy, cholecystectomy, and exploratory laparotomy. - Dr. Maria Carmela Villania-Mamauag is a board certified diplomate of the Philippine Pediatric Society with a degree of Doctor of Medicine from Our Lady of Fatima University, Valenzuela City and a Bachelor in Science in Psychology from Saint Louis University, Baguio City which was augmented by a year of Bachelor in Science in Family Life and Child development at the University of the Philippines, Diliman, Quezon City.
 Dr. Maria Carmela Villania-Mamauag is a board certified diplomate of the Philippine Pediatric Society with a degree of Doctor of Medicine from Our Lady of Fatima University, Valenzuela City and a Bachelor in Science in Psychology from Saint Louis University, Baguio City which was augmented by a year of Bachelor in Science in Family Life and Child development at the University of the Philippines, Diliman, Quezon City.
Dr. Maria Carmela Villania-Mamauag is a board certified diplomate of the Philippine Pediatric Society with a degree of Doctor of Medicine from Our Lady of Fatima University, Valenzuela City and a Bachelor in Science in Psychology from Saint Louis University, Baguio City which was augmented by a year of Bachelor in Science in Family Life and Child development at the University of the Philippines, Diliman, Quezon City. - Dr. Christina Johns is the vice-president of Communications at PM Pediatrics, a specialized pediatric urgent care provider. The pediatric emergency physician did her education at Johns Hopkins University School of Medicine and has over 25 years experience in the field.
 Dr. Christina Johns is the vice-president of Communications at PM Pediatrics, a specialized pediatric urgent care provider. The pediatric emergency physician did her education at Johns Hopkins University School of Medicine and has over 25 years experience in the field.
Dr. Christina Johns is the vice-president of Communications at PM Pediatrics, a specialized pediatric urgent care provider. The pediatric emergency physician did her education at Johns Hopkins University School of Medicine and has over 25 years experience in the field.
Read full bio of Dr Bisny T. Joseph
Read full bio of Dr. Ritika Shah
Read full bio of Ghazia Shah