Image: Shutterstock
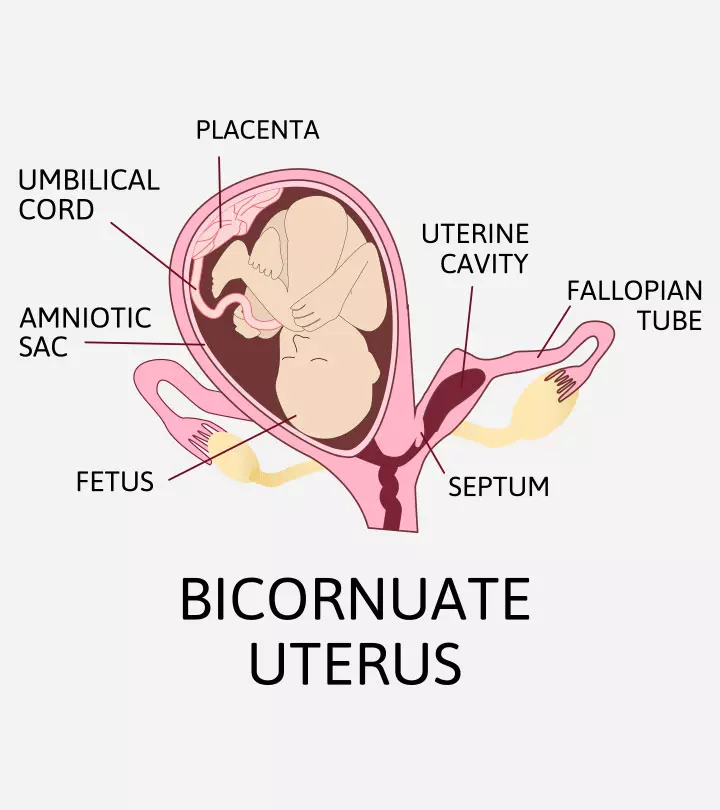
Bicornuate uterus (BU) is a congenital uterine abnormality or a Mullerian duct anomaly where the uterus (womb) is heart-shaped and has two horns. The uterus is normally pear-shaped, but the partial fusion of the Mullerian ducts (analogs of female reproductive organs) in the developmental phase can give rise to the heart shape. The bicornuate uterus may compromise nearly 10-39% of Mullerian duct anomalies. There are two types of anomalies depending on the partition of the cervix–bicornuate unicollis (partial bicornuate) and bicornuate bicollis (complete bicornuate). Women with a bicornuate uterus can have adverse pregnancy outcomes, including repeated pregnancy loss and preterm birth (1) (2). Read on to know the causes, symptoms, diagnosis, complications, and treatment of the bicornuate uterus.

Key Pointers
- A bicornuate uterus is a uterine abnormality present from birth and is referred to as a heart-shaped womb.
- DysmenorrheaiPainful periods caused by uterine contractions that may or may not be due to an underlying medical condition , repeated miscarriages, and pain in the abdomen are some symptoms associated with this anomaly.
- It might not affect a woman’s fertility but can result in fetal loss, malpresentation, preterm birth, etc.
Can You Get Pregnant With A Bicornuate Uterus?
Although the bicornuate or two-horned uterus was previously thought to be associated with infertility, recent studies do not confirm the association between bicornuate uterus and infertility. Most women with a bicornuate uterus can conceive; however, having a bicornuate uterus can put you at high risk for certain adverse pregnancy outcomes, thus requiring additional monitoring.
Sometimes, infertility, intrauterine fetal death, or threatened miscarriage may occur in women with bicornuate uterus due to other reasons. In many cases, doctors may have an incidental finding of a bicornuate uterus while looking for the probable causes of infertility or pregnancy loss. In fact, successful pregnancies of women with a bicornuate uterus and without correction surgeries or cerclage indicate that the bicornuate uterus itself is not a cause of infertility (1).
A blogger and mother ‘Smashleybebe’ shares how she learned that she has a bicornuate uterus. She says, “I was taking a bath just a few minutes ago and I started wondering if baby number 2 (if ever conceived) would come early like Calvin. Then I remembered something my doctor had said when he was delivering Calvin – he said it was no wonder Calvin was breech because I had a heart shaped uterus. He didn’t sound alarmed or anything and went on his merry way, and I never thought to research it to even see what my uterus looked like. Until today. The medical term for my uterus is Bicornuate Uterus (i).”
What Causes Bicornuate Uterus?
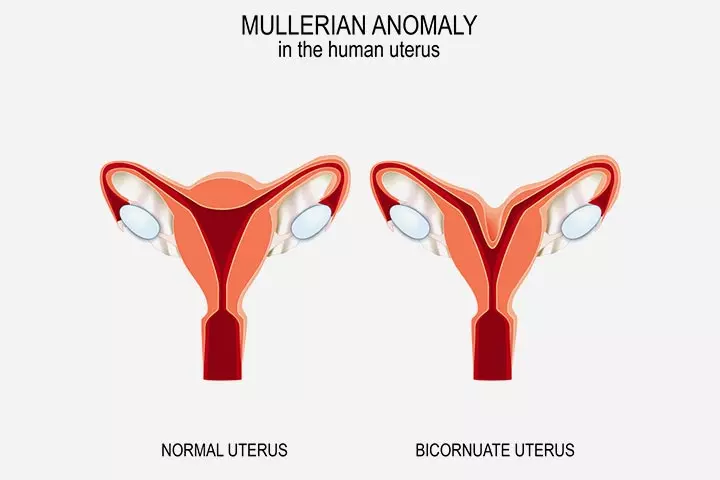
The cause of malformation in Mullerian ducts, including the bicornuate uterus, is not well understood. In fact, bicornuate uterus is one of the most frequently seen Mullerian duct anomalies. The American Society for Reproductive Medicine (ASRM) 2025 and MAC2021 (Müllerian Anomalies Classification 2025) defines bicornuate uterus as the uterus having an external fundal indentation depthiThe measurement that shows how deep the indentation is at the top of the uterus (called fundus) when looking at an ultrasound. of >1.0cm (10 mm) (10) (4). Genetic and environmental factors might play a role. Several studies showed that uterine anomalies are due to abnormal gene expression that occurs at birth, which means it is congenital (9). In addition, exposure to environmental factors, such as certain chemicals and drugs, can interfere with early fetal development, causing uterine anomalies, such as bicornuate uterus in female babies (3).
 Quick fact
Quick factWhat Are The Symptoms Of A Bicornuate Uterus?
Most women with bicornuate uterus may not have any symptoms and will not know they have the uterine anomaly until they undergo ultrasound or other imaging.
The following symptoms can be present in some women (3):
- Painful periods
- Abdominal pain
- Dyspareunia (pain during sex)
- Repeated miscarriages or pregnancy loss
- Irregular bleeding (rare)
A bicornuate uterus is associated with a longitudinal vaginal septum in 25% of cases. This can cause obstructive symptoms or pain during sex. The vaginal septum can also cause the inability to control menstrual bleeding with tampons (3).
Double cervix and uterus can be present in many women who bleed through tampons. Genital system and urinary track embryologic formation share common steps. For these reasons, we have to look for coexisting renal (kidney or ureter) abnormalities that may cause symptoms such as pelvic pain and urinary retention.
 Did you know?
Did you know?When To See A Doctor?

It is recommended to seek a gynecological consultation for any menstrual irregularities. You may also seek medical care for repeated pregnancy loss and infertility problems.
Seek care from infertility specialists skilled in reproductive surgeries if you fail to conceive within one year of trying (six months if you’re older than 36 years). Surgical repairs can enhance fertility and pregnancy outcomes.
How Is The Bicornuate Uterus Diagnosed?
Imaging tests are standard for diagnosing bicornuate uterus. The external uterine borders can be concave or heart-shaped, and the uterine horns look prominent on the images. The fundal cleft is more than one centimeter deep, and the intracorneal distance is wider.
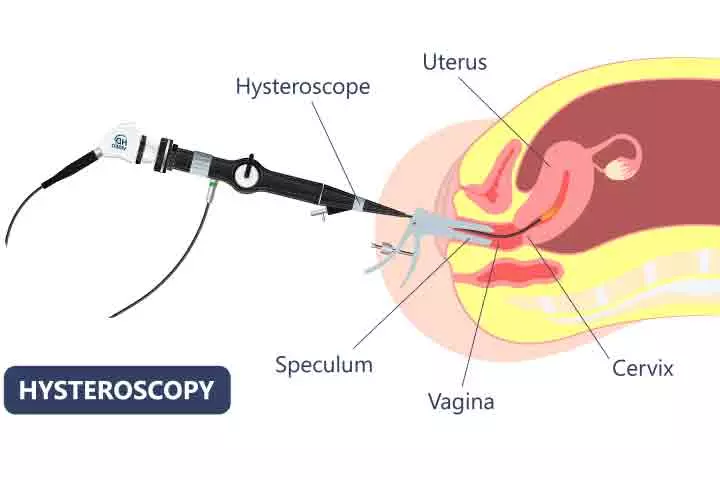
The diagnostic tests for bicornuate uterus include (4) (5):
- Pelvic examination in case of suspected symptoms. It will help identify the vaginal septum if present.
- Classic ultrasound imaging (sonography) helps visualize the uterus shape suggesting the condition. New 3D vaginal probes give an exact image of the malformation.
- Diagnosis hysteroscopy with the introduction of a camera inside the uterus will show the septa separating the two cavities
- Hysterosalpingogram (HSG) can visualize the divided uterus. However, the accuracy is 55% since the septate and bicornuate anomalies may appear similar. The angle of more than 105° indicates a bicornuate uterus, and less than 75° is a septate uterus. It is an old way to visualize the malformation.
- Magnetic resonance imaging (MRI) also helps visualize the uterus’s anatomy and the depth of fungal cleft and intercornual distances. The abnormality is indicated by the fundal cleft of more than 1cm and intercornual distance of more than 4cm.
How Is The Bicornuate Uterus Treated?
Surgical correction is recommended for women with bicornuate uterus and fertility problems. History of recurrent pregnancy loss and reproductive health issues without any cause of infertility indicates a surgical correction of the bicornuate uterus.
Cervical cerclage increases the fetal survival rate if the woman has coexisting cervical incompetence (cervical insufficiency). This procedure involves various sutures on the cervix to prevent pregnancy loss due to cervical insufficiency. In addition, doctors may suggest prophylactic cervical cerclageiA procedure of stitching and closing a weakened cervix during pregnancy to avoid preterm delivery for some women since the association between cervical incompetence and the bicornuate uterus is high. Vaginal and uterine septums are also surgically resected by operative hysteroscopy.
Strassman metroplasty, urethroplasty, or hysteroplasty is the corrective surgery for the bicornuate uterus. This procedure helps to fuse the bi-uterine cavity and the fundus. Pregnancy outcomes can be improved after the procedure (5).
 Point to consider
Point to considerWhat Are The Complications Of Bicornuate Uterus?
Common adverse pregnancy outcomes in women with bicornuate uterus may include (3):
- Fertility problems: Approximately 15-25% of women with uterine anomalies can have fertility and reproductive system issues. There is an increased risk for abnormal placentation, poor fetal growth, and ectopic pregnancies with a bicornuate uterus.
- Recurrent pregnancy loss or miscarriage: can be due to reduced uterine capacity or irregular uterine contractions from the abnormal shape.
- Fetal deformities: Congenital disabilities such as fetal limb deformity can be seen in some cases due to prolonged pressure on the limbs from space constraints in the uterine horn.
- Malpresentations: Lack of space for rotation may cause fetal malpresentation in many women with bicornuate uterus. In some cases, the cephalic presentation occurs if the fetus turns at the beginning of the third trimester and maintains the position until term.
A mother diagnosed with a Bicornuate Uterus at the age of fifteen recounts her fourth pregnancy journey when she delivered a preterm baby. She states, “Baby number two, pregnancy number four, decided to stay put for some time. I had steroids at 28 weeks to strengthen his (her fetus’) lungs in case he tried to copy his brother, but this time he became a breach! “He stayed that way until 35 weeks when his growth slowed down. So, Michael (her son) was born at 35 weeks via C-section (ii).”
- Preterm birth: Cervical incompetence may result in early delivery if the cervical cerclage is not placed. However, there are cases of successful singleton and twin pregnancies without cerclage, and the outcomes may vary for each woman. This is common if the cervical length is less than 25mm on transvaginal ultrasound.
- Postpartum hemorrhage: Severe postpartum bleeding may occur if the bicornuate uterus does not contract after delivery. However, surgical and nonsurgical alternatives such as suturing or ligating the blood vessels or Bakri balloon may help reduce the bleeding.
- Pregnancy-induced hypertension: Women with coexisting renal and uterine anomalies may have a higher risk of high blood pressure in pregnancy. During pregnancy, frequent monitoring of the blood pressure may help identify and control the pressure before developing complications.
- Uterine rupture: The presence of fibrous bands or abnormal development of the lower part of the uterus (corpora) can increase the risk for rupture even in first-time pregnant women.
- Urinary tract anomalies: Many women with uterine anomalies have coexisting urinary tract anomalies such as renal agenesis or pelvic kidney.
- Placental abnormalities: The condition also increases the risk of placental abnormalities and associated complications, such as placental abruption.
- Fetal position: A bicornuate uterus can also lead to complications with fetal positioning during delivery.
- Undetected endometrial cancer: A bicornuate uterus is not an independent risk factor for developing endometrial cancer. However, cancer may go undetected if samples are collected from the healthy part of the uterus. Delay in detection and treatment can worsen the prognosis.
Can You Have Twins With A Bicornuate Uterus?
It is possible to have twin pregnancies with a bicornuate uterus. However, twin pregnancies have a higher risk of complications in women with uterine malformations. Preterm birth and low birth weight are common twin pregnancy complications in women with a bicornuate uterus and other uterine malformations. Cervical cerclage and vaginal progesteroneiA steroid hormone that plays an important role in the regulation of the menstrual cycle and early stages of pregnancy may help prevent preterm delivery (6).
Frequently Asked Questions
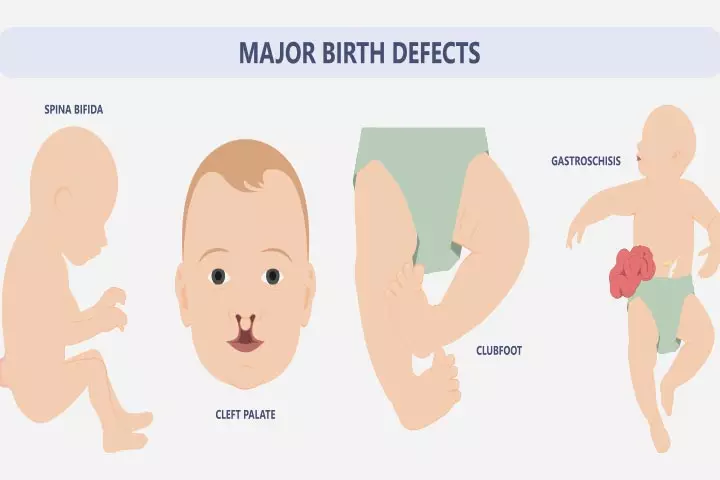
1. What congenital disabilities can a bicornuate uterus cause?
A study showed that babies of mothers with a bicornuate uterus had a four times higher risk for congenital disabilities than infants born to women with a normal uterus. Specific anomalies such as limb deficiencies, nasal hypoplasiaiA condition where the sonography results show that fetal nasal bone length is less than normal , omphaloceleiA rare congenital condition causing abdominal organs to protrude outside the body through the abdominal wall , and teratomas were more closely associated (7).
2. Can a bicornuate uterus be fixed?
Frequent prenatal screening is recommended if a woman is diagnosed with a bicornuate uterus during an ongoing pregnancy. If a non-pregnant woman is diagnosed, the condition may be surgically corrected using Strassman metroplasty. A laparoscopic approach is preferred to reduce the risk of bleeding and infections (3).
3. Can I go for IVF with a bicornuate uterus?
Yes, women with bicornuate uterus may have a successful pregnancy with in-vitro fertilization (IVF). A study reports that ovarian responses and pregnancy outcomes are not significantly different in women with no diagnosis of the bicornuate uterus and undergoing IVF treatment (8).
Infographic: Bicornuate Uterus Pregnancy Care
Pregnancy with a bicornuate uterus is included in the high-risk group due to the possible prenatal, natal, and postpartum complications. Go through the infographic to learn about pregnancy care for women with bicornuate uterus.
Some thing wrong with infographic shortcode. please verify shortcode syntax
This video gives valuable insight into the bicornuate uterus and its effect on the conceiving ability of a person by an expert. To learn more watch this video.
A bicornuate uterus is a structural anomaly of the uterus. Some women may develop symptoms and complications, while a few can be asymptomatic. The chances of conceiving and continuing a pregnancy to the term also vary in each woman. You may consult the doctor and undergo correction surgeries if needed to enhance your reproductive outcomes.
Personal Experience: Source
MomJunction articles include first-hand experiences to provide you with better insights through real-life narratives. Here are the sources of personal accounts referenced in this article.
i. Heart shaped baby house.https://calvintsmom.wordpress.com/2015/01/10/heart-shaped-baby-house/
ii. A heart shaped uterus: A funny shape, but really not that funny.
https://yummymummysblog.wordpress.com/2015/08/28/a-heart-shaped-uterus-a-funny-shape-but-really-not-that-funny/
References
- Adewale Samson Adeyemi et al.; (2013); Successful pregnancy in one horn of a bicornuate uterus.
https://journals.lww.com/aoam/fulltext/2013/12040/successful_pregnancy_in_one_horn_of_a_bicornuate.10.aspx - Ibrahim Haruna Gele et al.; (2025); Bicornuate Uterus Presenting with Recurrent Pregnancy Loss; the Role of Hysterosalpingography in the Diagnosis: A Report of Two Cases.
https://www.ijhsr.org/IJHSR_Vol.10_Issue.12_Dec2020/38.pdf - Parneet Kaur and Deepan Panneerselvam; Bicornuate Uterus.
https://www.ncbi.nlm.nih.gov/books/NBK560859/ - Mullerian Anomalies.
https://www.pennmedicine.org/for-patients-and-visitors/patient-information/conditions-treated-a-to-z/mullerian-anomalies - Bicornuate uterus.
https://radiopaedia.org/articles/bicornuate-uterus - Katherine Adams and Lee Minuzzo; (2019); Successful delivery of spontaneously conceived twins in a single horn of a bicornuate uterus: A case report.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6401982/ - M L Martinez-Frías et al.; (1998); Congenital anomalies in the offspring of mothers with a bicornuate uterus.
https://pubmed.ncbi.nlm.nih.gov/9521976/# - Wei-Ya Kong et al.; (2025); Effects of bicornuate uterus on pregnancy and obstetric outcomes of in vitro fertilization / intracytoplasmic sperm injection.
https://pubmed.ncbi.nlm.nih.gov/33421810/# - Bicornuate Uterus.
https://my.clevelandclinic.org/health/diseases/22798-bicornuate-uterus - Samantha M. Pfeifer et al.; (2025); ASRM mullerian anomalies classification 2025.
https://www.asrm.org/globalassets/_asrm/practice-guidance/practice-guidelines/pdf/mac2021_manuscript.pdf
Community Experiences
Join the conversation and become a part of our nurturing community! Share your stories, experiences, and insights to connect with fellow parents.
Read full bio of Dr. Ben Abbes Taarji Hicham
Read full bio of Dr Bisny T. Joseph
Read full bio of Rebecca Malachi
Read full bio of Reshmi Das