Image: ShutterStock
After delivery, your body discharges lochia, a menstrual period-like discharge consisting of blood, uterine tissues, and mucus, for four to six weeks. Lochia may also contain blood clots. Blood clots after birth usually form because the blood flow rate due to uterineiInability of the uterus to contract sufficiently during or after childbirth, leading to excessive bleeding. wall shedding is higher than blood flow out of the body, causing the blood to collect in the uterus. Generally, the presence of a few plum-sized blood clots in postpartum discharge, especially in the first few days after delivery, is normal (1). However, if you notice too many clots or the clots are big, it may indicate an underlying problem. Continue reading as we tell you more about blood clots in the vaginal discharge, its risks, and tips on preventing blood clots after delivery.

Key Pointers
- During the initial days after delivery, small blood clots in the postpartum discharge are normal.
- The discharge of clots will decrease and change in color and amount over time.
- The time of day, breastfeeding, and exercise can impact blood loss and clot size.
- Blood clots post-childbirth are diagnosed with a combination of tests depending on the severity of the clots.
- Treatment for blood clots ranges from compression stockings to specific interventions for severe conditions.
- Measures to prevent blood clots include staying active, informed, hydrated, and being aware of the risk factors and symptoms.
Are Blood Clots Normal Post Delivery?
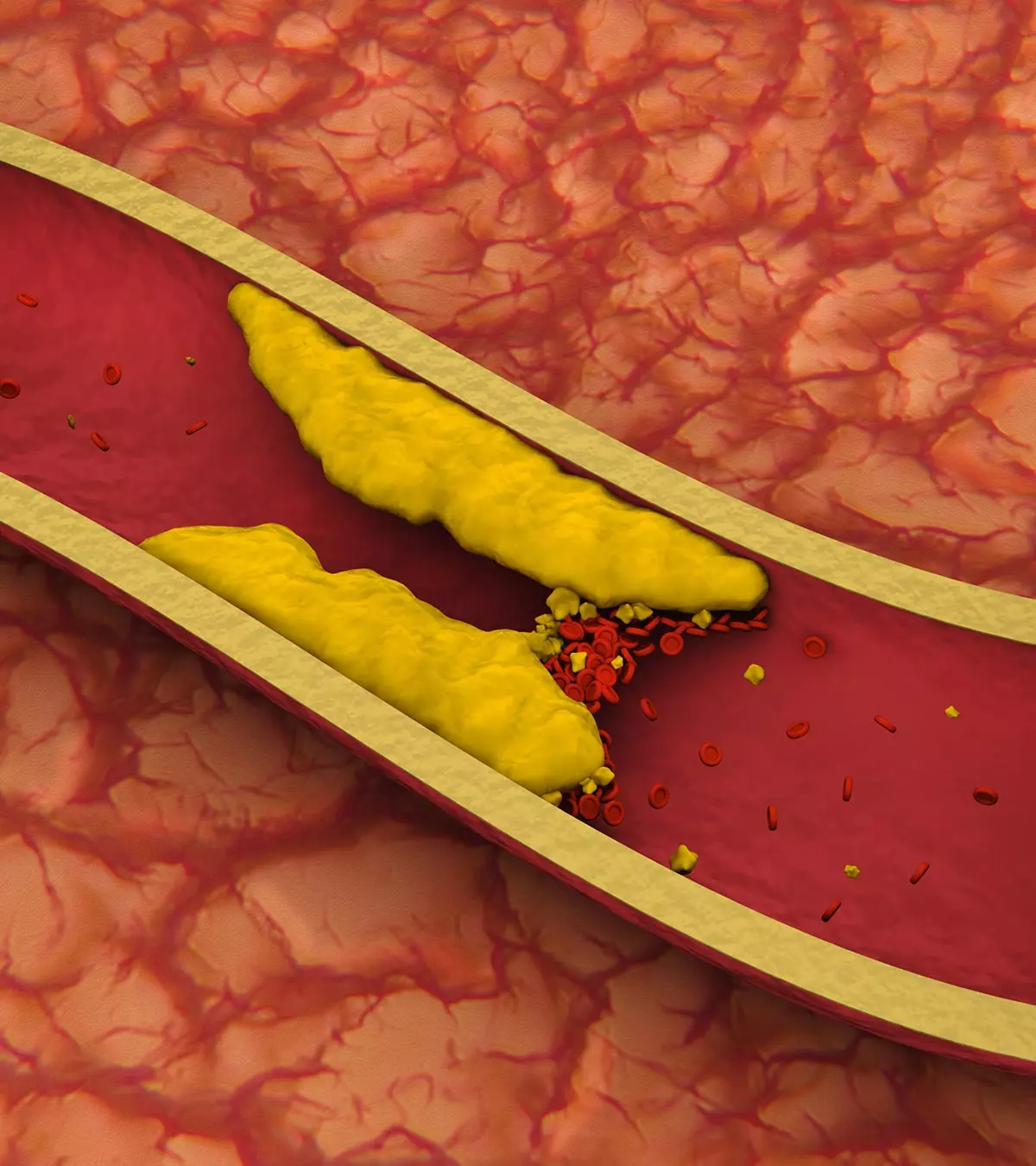
A blood clot is a mass of blood sticking together to form a jelly-like substance. Passing a few small blood clots is common after delivery. These clots reduce in size and frequency of appearance as the days pass (2). If you notice anything otherwise, seek prompt medical attention to avoid complications such as uterus atonyiInsufficient uterine contraction following childbirth , uterus rupture, tears in the vagina and cervix during delivery, preeclampsiaiA pregnancy disorder characterized by high blood pressure, water retention, and protein content in urine. , pieces of placenta which have remained inside the uterus after delivery, deep vein thrombosisiA condition marked by the development of blood clots within the deep veins, particularly in the legs. or pulmonary embolismiA condition in which a blood clot (originating from elsewhere in the body) blocks blood flow in the lungs. .
What Are The Symptoms Of Normal Blood Clotting After Childbirth?
Coagulation or clotting is common after childbirth, and the amount discharged will reduce eventually. Here is a guide to help you understand the discharge of blood for up to six weeks post-delivery (3).
| Days/Weeks after delivery | Color of blood | Amount discharged |
|---|---|---|
| First day | Fresh red or brownish red blood. | Considerably heavy loss of blood, soaking the napkins every few hours. You may pass one or two large clots about the size of a tomato. The smaller one may be about the size of a grape. |
| Days 2-6 | Dark brown or pinkish red blood. | Moderate amount of blood loss with the stain measuring 7-12cm on a sanitary pad. Very small clots will be passed once or twice in a day. |
| Days 7-10 | Color stays the same or may appear light brown or pinkish red. | Amount of blood loss reduces significantly, without soaking the pad as profusely as earlier. The stain on a sanitary pad measures less than 7cm. |
| Days 11-14 | The color gets much lighter. If you are very active, then it may stay a little bright. | The amount of blood is reduced by a degree, hardly staining the sanitary pad. |
| 3rd -4th weeks | Blood loss may still be there, with a paler tint or in creamy white color. | There will be very little or no blood loss at all. If the blood loss stops after three or four weeks and fresh blood flow begins, it could indicate the return of your menstrual cycle if mother has stopped breast feeding |
| At about six weeks | Occasional blood loss that is either brown, pinkish red, or creamy yellow. | A light, pale stain on the sanitary pad that may continue either throughout the day or on some days. |
The color and size of the blood clots after birth and the amount of blood loss may be affected by the following factors:
- Time of the day: The blood loss can be high in the mornings as the blood pools in the uterus when you lie down and flows down into the vagina when you stand up.
- Breastfeeding: Release of the oxytociniA chemical messenger and hormone involved in childbirth, lactation, and social bonding. hormone during breastfeeding, which is one of the postpartum hormones, also triggers the contraction of the uterus with or without pain. It is followed by a slight increase in the discharge of lochia.
- Exercising: Gentle physical activities such as walking can also cause a heavy blood loss during the first two weeks post delivery.

If the blood clots are different than they usually are post-delivery, consult your doctor.
What Are The Symptoms Of An Abnormal Blood Clot?
Abnormal blood clotting could indicate deep vein thrombosisiThe development of a blood clot (thrombus) in a deep vein, usually in the legs (DVT). If left untreated, it could lead to a life-threatening complication called pulmonary embolismiA lung artery becomes blocked unexpectedly (PE). According to a study, the incidence of postpartum pulmonary embolism occurring without a prior thrombotic event was 0.45 per 1,000 births (4). DVT and PE are treatable and preventable, when discovered early (5). Therefore, look out for the symptoms of a dangerous blood clot (6):
For deep vein thrombosis (DVT)

- Swelling (in one leg or arm or pelvic area)
- Reddish or bluish skin discoloration
- Leg pain or tenderness often described as a cramp or Charley horse
- Leg or arm feels warmer on touch
Care Connely, a mother of two, recounts her encounter with blood clots a day after giving birth. She says, “I woke up in the middle of the night with pain in my left calf. I was like, what is this? So I Google it, and of course, the first thing that comes up is after you have a baby, you can get a blood clot in your calf, and it’s usually the left calf. So it still hurts, like I didn’t pull it. It felt like I pulled it, a real dull, light pain in the middle of my calf (i).”
After consulting a midwife, she decided to seek medical attention. An ultrasound confirmed the presence of a blood clot in her calf. This personal account highlights the importance of being vigilant about postpartum symptoms that could indicate a blood clot.
If you notice any such symptoms, contact your doctor. However, you can have pulmonary embolism without any symptoms of deep vein thrombosis. Therefore, it is wise to check for the following symptoms as well:
For pulmonary embolism
- Shortness of breath
- Sharp or stabbing chest pain that may worsen when you take a deep breath
- Rapid heart rate
- An unexplained cough with or without bloody mucus
Apart from a recent delivery, there are some other factors that increase the risk of DVT and pulmonary embolism (7):
- Previous blood clots
- A family history of blood clotting disorders
- Acquired thrombophiliaiA condition characterized by the tendency of the blood to form clots easily.
- Medical co-morbidities (sickle cell anemia, SLE, nephrotic syndrome, inflammatory conditions
- Maternal obesity
- Increased maternal age (over 35 years)
- Prolonged immobility (like bed rest or long distance travel)
- Multiple pregnancies
- Any medical condition like cancer or infections
- Dehydration
- Preeclampsia
- Prolonged labor
- Mid cavity rotational forceps delivery
- Postpartum hemorrhage
If pulmonary embolism is not treated, it could turn fatal. Timely diagnosis and treatment could avoid further complications. As per studies, without treatment, acute pulmonary embolism can lead to death in up to 30% of cases, while proper diagnosis and treatment reduce the mortality rate to 8% (8).
How Are Blood Clots After Childbirth Diagnosed And Treated?
If DVT or pulmonary embolism is suspected postpartum, the doctor will suggest a few diagnostic tests before prescribing the ideal course of treatment (9) (10).
Diagnosis
- D-dimer test: In the case of a suspected deep vein thrombosis, ultrasonography is done. Then, a blood test is carried out to detect the amount of D-dimer, which is a substance released from the blood clots. An abnormally high D-timer amount indicates that blood clots are circulating in the bloodstream.
- CT scan: Computed tomography (CT) of the chest is carried out to detect pulmonary embolism. It is carried out after injecting a radiopaque contrast agent, which is a form of a dye, into the vein. The dye helps in clearing any blockage to give clear visibility inside the vein.

Apart from CT scan, a doctor might also prescribe for:
- Ventilation-perfusion scan: Also known as V/Q scan or isotope lung scanning, it is prescribed to examine the flow of air and blood in the lungs. A part in the lungs with air in it but with no blood supply is indicative of pulmonary embolism (11).
Once the clot is diagnosed, prompt treatment is crucial. Depending on the severity of risk a clot could pose, the treatment plan is formed.
Treatment
The course of treatment would be suggested as per the severity of the condition (11):
- Compression stocking: If you are suffering from pain and swelling, compression stocking is a likely part of the treatment to provide symptomatic relief.

- Anticoagulant drugs: Anticoagulants are generally used for treating postpartum blood clotting disorders. Women diagnosed with blood clots need to take this medication for six weeks post delivery (12). The treatment is likely to start with an injection of HepariniA blood-thinning medication, or anticoagulant, works by preventing new blood clots from forming and limiting the growth of existing ones . It is injected through the vein or under the skin for the first five to ten days. Post that, oral drug therapy begins and includes medications such as warfarin, edoxaban, rivaroxaban, apixaban, and dabigatran.
Lindsay, a mother, recalls her experience of being diagnosed with a massive blood clot (Deep Vein Thrombosis or DVT) in her Inferior Vena Cava, which was detected through a CT scan. She received treatment and was prescribed blood thinners. She shares, “Before we left, we would be taught how to administer blood thinners via an injection. If I wanted to continue breastfeeding, I would have to receive my blood thinners this way. At the last minute, I decided that I would prefer to take an oral blood thinner. Injecting myself twice a day with the likelihood of needing Michael’s (husband) help felt like too much to deal with (ii).”
- Thrombolytics: These are the drugs used to dissolve the clots. They basically break large clots into smaller ones, thereby reducing the risk of further complications. They are used in serious cases of pulmonary embolism.
- Inferior vena cava filter: This procedure is used in the cases where anticoagulants cannot be used or don’t work well. A filter is inserted inside the inferior vena cava (a large vein that brings blood back to the heart). This traps the clot before it reaches the lungs.
- Thrombectomy/ embolectomy: Embolectomy is a surgical procedure used for patients suffering from pulmonary embolism. The procedure involves removal of the blockage in the lungs caused by the clot.
While you are undergoing treatment for blood clots, it is wise to consult your doctor about the safety of breastfeeding.
 Did you know?
Did you know?How To Prevent Blood Clots After Childbirth?
Here are some tips you can follow to prevent any blood clotting risks after a cesarean section or natural delivery (13):
- Be aware of the risk factors for blood clotting.
- Stay active and keep moving regularly. Walking is the best activity postpartum.
- Stay informed about the family history of this disorder.
- Ensure that the doctor knows about your family history of blood clotting disorders.
- Drink plenty of fluids to stay hydrated. Dehydration is one of the causes of DVT.
- Always look out for any symptoms of a blood clot.
- Do not use tampons for at least six weeks after delivery.
- Maintain good health and overall well-being by following a balanced diet.
How To Care For Yourself?

Here are some tips you can follow in case of excessive blood flow:
- Stock up on sanitary pads for this period and avoid using tampons.
- Keep your bladder empty as it helps in contracting the uterus and aids in reducing postpartum bleeding.
- Wear compression stockings, if they are recommended to you.
- Follow a healthy lifestyle. This includes eating healthy, exercising, and quitting smoking (if you smoke).
- If you are planning to travel after the treatment, check once with your doctor. Ideally, it is advised to avoid long journeys until at least two weeks after starting anticoagulants.
- Rest as much as you can.
By following some basic steps you can prevent blood clots. However, after delivery, there are some symptoms that could indicate some issue.
 Point to consider
Point to considerWhen To Call The Doctor?
If you notice any of the following symptoms, call your doctor immediately (1).
- Fever over 100.4 degree fahrenheit with severe chills.
- A blood flow that needs you to change the pad per hour.
- Large size blood clots: If you continue to pass large size blood clots after the first 24 hours of delivery, following heavy blood loss.
- Heavy blood flow: The blood flow should reduce gradually as the week passes. If it does not, call the doctor.
- Foul smell: If the vaginal discharge has an offensive odor, which could be due to an infection of the uterus or the perineumi A layer of skin present between the genitals and anus (inside the thighs) in females. .
- Pelvic pain: A urinary infection, infection of the uterus, or constipation can cause pelvic pain.
- Other important symptoms such as: Blurred vision, severe headache and fainting, chills, rapid heartbeat, weakness, dizziness, swelling around the pelvic area or in the leg and difficulty breathing.
Timely diagnosis, treatment and prevention can possibly help you get through any serious risks that blood clots pose.
 Caution
CautionDoes C-Section Increase The Risk Of Blood Clots?
Recent studies revealed that women undergoing a c-section were at a higher risk of developing dangerous postpartum blood clots compared to those who delivered vaginally. The risk was especially high in cases of an emergency c-section (14). According to a study by the Duke University School of Medicine, venous thromboembolism (VTE) is prevalent among 2.1 women per 1,000 hospitalizations following cesarean delivery at 330 days after delivery (15).
According to Dr. Marc Blondon, of Geneva University Hospital in Switzerland, there is an increase in the blood’s susceptibility to clotting during surgery. Thus, women who are considered for a c-section without any medical indication for it, are at higher risks. However, the risk remains low in the majority of women who had undergone a c-section.
The American College of Obstetricians and Gynecologists says that for women with no risks of a blood clot, a pneumatic compression device should be used before delivery. This helps reduce any potential risks. This device is placed on the legs to prevent blood from pooling inside the calves (16).
Frequently Asked Questions
1. Can massage break up blood clots?
Your healthcare provider can massage the uterus to encourage contraction, minimize bleeding, and aid with the body’s ability to pass blood clots (17).
2. Why do I need blood thinners after giving birth?
Blood thinners stop the growth and production of blood clots. In the six weeks following the delivery of the child, a woman is at a high risk of developing blood clots. Therefore, women with clotting issues may be advised to restart their anticoagulation therapy soon after delivery and continue it for at least six weeks. For women at low risk of developing clots, the healthcare provider will advise the suggested duration of anticoagulants (18).
3. Are certain women more at risk of developing blood clots after giving birth?
Yes, some women face an elevated risk of developing blood clots after childbirth. Factors that raise this risk include prior clots, genetic predisposition, obesity, extended periods of inactivity, multiple births, advanced maternal age, and other medical conditions such as cancer or infection (6).
4. Can a woman with a blood clot after giving birth breastfeed her baby while taking blood-thinning medication?
Women must consult their healthcare provider regarding the compatibility of breastfeeding with blood-thinning medication. Personalized guidance can be provided based on the medicine, medical history, and potential risks and benefits.
5. Can a woman with a history of blood clots take hormonal contraceptives after giving birth?
It’s crucial for a woman who has had blood clots in the past to consult her healthcare provider before contemplating hormonal contraceptives postpartum. They can evaluate the risks and advantages, considering her medical background, and offer suitable advice.
If you have delivered recently, stay informed about the changes in your body. If you notice anything unusual, there is no harm in consulting a doctor. Getting the clots treated on time, with the right medications can keep you away from possible life-threatening complications they might lead to.
Infographic: Who Needs An Inferior Vena Cava (IVC) Filter In Pregnancy?
Inferior vena cava (IVC) filters are often placed during pregnancy and up to six weeks postpartum to prevent blood clots in the lower body from moving to the lungs. It is useful if the mother has limited mobility after delivery. Go through the infographic to know indications to place IVC filters during pregnancy and postpartum.
Some thing wrong with infographic shortcode. please verify shortcode syntax
Postpartum bleeding is a normal part of the recovery process. Learn how long it should last and what to expect during this time, from this video
Personal Experience: Sources
MomJunction articles include first-hand experiences to provide you with better insights through real-life narratives. Here are the sources of personal accounts referenced in this article.
i. Three-week-old baby update + Postpartum story time – Surviving blood clots 3 weeks postpartum + Newborn;
https://www.youtube.com/watch?feature=shared&v=HkBfBA-JZ4o
ii. Lindsay’s Story: Postpartum Blood Clot and Pulmonary Embolism;
https://thebirthtraumamama.com/postpartum-blood-clot-and-pulmonary-embolism/
References
- Pregnancy: Physical Changes After Delivery; Cleveland Clinic
- Blood loss after birth.; Queensland Clinical Guidelines; State of Queensland
- Bleeding after birth: 10 things you need to know; NCT
- MORRIS, J., ALGERT, C., & ROBERTS, C.; Incidence and risk factors for pulmonary embolism in the postpartum period; Journal of Thrombosis and Haemostasis
- About Venous Thromboembolism (Blood Clots); Centers For Disease Control And Prevention
- Blood Clot Info: Risks, Symptoms, And Prevention; National Blood Clot Alliance
- Blood Clotting & Pregnancy; American Society of Hematology
- Bĕlohlávek, J., Dytrych, V., & Linhart, A. Pulmonary embolism, part I: Epidemiology, risk factors and risk stratification, pathophysiology, clinical presentation, diagnosis and nonthrombotic pulmonary embolism; Experimental & Clinical Cardiology
- Pulmonary embolism: Symptoms, causes, risk factors, and treatment; Harvard Health Publishing
- How is a pulmonary embolism diagnosed?; Pulmonary embolism; British Lung Foundation
- Testing and Diagnosis for Venous Thromboembolism; Centers For Disease Control And Prevention
- Pregnancy and Childbirth; Women and Blood Clots
- Pulmonary Embolism; Medline Plus; U.S National Library of Medicine
- Cesarean section carries increased risk for postpartum venous thromboembolism (VTE); Science Daily
- Federspiel, Jerome J., et al.; Venous Thromboembolism Incidence among Patients Recommended for Pharmacologic Thromboembolism Prophylaxis After Cesarean Delivery in Selected Guidelines; Journal of Thrombosis and Haemostasis
- DVT Prevention: Intermittent Pneumatic Compression Devices; Johns Hopkins Medicine
- Postpartum hemorrhage; March of Dimes
- Pregnancy and Post Childbirth;Women and Blood Clots
- The Truth About Blood Thinners, Leafy Greens, And Vitamin K; The Trustees of the University of Pennsylvania
Community Experiences
Join the conversation and become a part of our nurturing community! Share your stories, experiences, and insights to connect with fellow parents.
Read full bio of Dr. Irene (Eirini) Orfanoudaki
Read full bio of shreeja pillai
Read full bio of Rebecca Malachi
Read full bio of Reshmi Das