Image: iStock
Colds and several other respiratory infections fall under common diseases in children. Children usually contract common childhood illnesses, such as sore throat, skin infections, and ear infections at some point. Although curable, a few diseases might result in complications, morbidity, and mortality if diagnosis and treatment are delayed. Thus, parents and caregivers must be aware of common childhood illnesses to seek proper care on time.

The below post helps you understand the common childhood diseases, their symptoms, treatments, and preventive measures.
Key Pointers
- Common cold, cough, ear pain, skin, and urinary tract infections are common illnesses in children.
- You may follow certain home care tips such as practicing good hygiene, encouraging frequent handwashing, and avoiding allergen exposures in children.
- Furthermore, you may keep your child away from infected persons, vaccinate them as scheduled, and use safety equipment such as bathing cups to prevent infections.
- Seek medical care if your child’s symptoms worsen or stay for longer than usual to facilitate timely diagnosis and appropriate treatment for the condition.
Common Childhood Illnesses: Their Symptoms And Treatments
Being aware of the common childhood illnesses can help you understand what illness your child might be having and provide proper treatment.
Note: The information given in this post is for the sole purpose of making parents aware of the common illnesses in children. Seek a healthcare provider’s consultation or advice to diagnose and treat any illness in children.
According to the American Academy of Pediatrics (AAP), some of the most common childhood illnesses and their approved treatments are as follows (1).
1. Sore throat
A sore throat is an infection that causes pain and irritation to the throat, often felt as scratchiness. It is common in children, and the symptoms may often worsen while swallowing food. Various viruses and bacteria can cause this. Strep throat, caused by group A streptococcusi A type of bacteria responsible for many different major and minor infections , is highly contagious and can spread through respiratory droplets or contact with infected persons. A global meta-study by multiple researchers indicates that globally around 288.6 million children between the age of five and fourteen years are diagnosed with group A Streptococcus pharyngitis.
The common symptoms of sore throat may include (2).
- Pain
- Itchy or scratchy throat
- Swallowing difficulty
- Swollen neck glands
- Voice changes
- Pus or white patches on the tonsils
- Fever
- Cough
- Runny nose
- Body ache
- Sneezing
- Vomiting
In addition to the clinical features and physical examination, lab tests and rapid strep throat tests of throat swabs are done at the doctor’s office to diagnose strep throat. After the tests, children with strep throat receive antibiotic prescriptions.
It is necessary to take the prescribed course of antibiotics even though the symptoms improve or go away to avoid complications, such as rheumatic fever. Sore throats caused by viruses are not treated with antibiotics. Most children with viral strep throat get better in seven to ten days. Steroid medications are also not recommended for sore throat treatment.
 Point to consider
Point to consider2. Ear pain

Ear pain or earache is common in children, and this can be felt as sharp, burning, or dull pain in one or both ears. This is also one of the most common infant and newborn problems. Some children may have short-term pain, while others may have ongoing pain until the underlying condition is resolved.
The common symptoms associated with ear pain may include (3).
- Fever
- Irritability
- Jaw pain
- Pain while chewing
- Ear discharge that is often foul-smelling
- Hearing difficulties
- Itching
The common causes of childhood ear pain may include
- Middle ear infection (otitis media) caused by allergies, viruses, and bacteria
- Outer ear canal infection (otitis externa) or swimmer’s ear, which is usually caused when the water in the ear canal is not drained out well after swimming.
- Pressure in the ear due to cold or sinus infections
- Teeth pain radiating to the jaw and the ears
Treatments for ear pain in children may include the following.
- Ear pain with high fever can be due to a bacterial infection, and pediatricians may prescribe antibiotics.
- Antibiotic treatment with amoxicillin is often prescribed for middle ear infections. Other antibiotics are given only for children with allergies to penicillin and recurrent or chronic ear infections.
- Ear infections caused by viruses do not require antibiotics. Doctors may suggest applying a warm compress (warm cloth) over the affected ears to relieve pain in mild cases.
- Over-the-counter pain medications such as Tylenol (acetaminophen), pain-relieving ear drops, and decongestants are usually prescribed for severe ear pain due to viral infections.
Pediatricians may recommend office visits to observe a child’s ear using an otoscope for accurate diagnosis, as the symptoms alone may not be enough to determine the exact cause in many cases.
3. Urinary tract infections
Urinary tract infections (UTIs) can affect any part of the urinary system, including the urethra, bladder, ureter, and kidneys, and are often caused by the build-up of bacteria. A UTI may occur at any age, and girls are more vulnerable than boys due to the shorter length of the urethra (4).
Constipation and wiping the anal region in the wrong direction after toilet use can spread bacteria to the urethra in children. These infections usually spread from the lower urinary tracts to the upper tracts and further from the urethra to the kidneys. The common types of UTIs include
- Cystitis (bladder infection)
- Ureteritis (ureter infection)
- Pyelonephritis (kidney infection)
- Urethritis (urethra infection)
The following signs and symptoms are seen in UTIs in children.
- Pain or burning sensation while urinating
- Side or groin pain
- Abdominal pain or stomachache
- Back pain
- Fever
- Urgency to urinate
- Frequent urination
- Bedwetting (enuresis) in toilet trained children
Pediatricians usually order urine tests before prescribing medications. Antibiotic treatments for UTIs may vary according to the causative agents found in a child’s urine. Doctors may also suggest taking extra fluids and schedule follow-up visits to test the urine after treatment.
 Did you know?
Did you know?4. Skin infections

Skin infections are common in childhood and may affect any part of the body. Pediatric dermatologists may observe the skin infection and often order skin culture or biopsy of the skin swab to identify the exact causes. The following types of skin infections are usually seen in pediatric populations (5).
- Bacterial skin infections: These may include cellulitis (infection of the skin surface and underlying tissue), impetigo (strep or staph infection with blisters and scaling), and paronychia (infection around the nails).
- Fungal skin infections: These include paronychia and tinea infections (dermatophyte infection of the skin, nails, and scalp). Athlete’s foot (affects the skin between the toes and toenails), jock itch (tinea cruris) in kids (affects the groin and upper thigh skin), ringworm (circular rash anywhere on the skin) are common types of tinea infections in children. Yeast skin infections and skin rashes in children may include diaper rash in babies and toddlers, paronychia, and thrush (candida infection).
- Viral skin infections: These may include warts (small bumps due to HPV), herpes (sores and blisters), molluscum contagiosum (wart-like skin lesion), and other forms of viral rash in children.
- Erythema multiforme: This is a skin eruption with a target lesion that appears as a bull’s-eye-shaped rash. It may occur as a reaction to drugs and can be due to a bacterial, fungal, or viral infection.
The common symptoms of skin infection in children may include
- Skin rashes and eruptions (elevated bumps)
- Red, itchy skin
- Painful rashes
- Swelling of the affected skin (inflammation)
- Fever
- Rashes
The treatment options for skin infections may vary depending on the cause. Topical or oral antifungals, antibiotics, or antivirals are prescribed depending on the type of infection and severity. Most children respond well to the treatment, and the skin lesions may clear up in a few weeks. You may also apprise the doctors of the history of MRSA infections, staph infection, or other resistant bacteria in children or family members.
5. Bronchitis
Bronchitis is the inflammation of the bronchial tubeiMuscular tubes connecting the throat to the lungs linings in the lungs. Most children may have this infection for a short term (acute bronchitis). A long-term bronchial infection called chronic bronchitis is rare in children. Viruses, bacteria, and airway irritants can cause acute bronchitis in children.
Children with asthma, allergies, large tonsils or adenoids, and chronic sinusitis are more likely to develop bronchitis. Exposure to secondhand smoke can also increase a child’s risk (6).
The symptoms of bronchitis in children may include
- Dry cough or a productive cough (with sputum).
- Runny nose.
- Chest pain.
- Chills and mild fever.
- Chest congestion or tightness.
- Feeling unwell.
- Muscle aches.
- Wheezing.
- Sore throat.
- Vomiting.
Most of the bronchitis symptoms can last up to a week or two. However, the cough may continue for a few more weeks, even after the infection clears. Sputum samples, chest X-rays, and pulse oximetry can help diagnose bronchitis. Even though children may cough for more than eight or ten days, they may not require antibiotics.
Pediatricians may recommend plenty of rest, fluids, humidifiers, and cough, fever, and pain medications for children. Ibuprofen or acetaminophen are usually prescribed for fever and pain. Aspirin should not be given to children since it may cause Reye’s syndromeiA rare condition causing swelling in the brain and liver leading to diarrhea, vomiting, and severe weakness . Cough medications are also given with caution according to the child’s age and other factors.
6. Bronchiolitis

Bronchiolitis is the inflammation (swelling) of the smaller airways (bronchioles) in the lungs and is common in early spring and winter (cold and flu seasons). Children younger than two years are commonly affected by this condition. Preemies, babies who have not been breastfed, and children exposed to smoke are more likely to develop bronchiolitis (7).
Respiratory syncytial virus (RSV) is the most common cause of bronchiolitis. Rhinovirusi A virus responsible for causing the common cold, sore throat, and ear infections , adenovirusiA group of viruses that mainly cause fever, pink eye, pneumonia, and bladder infections in children , influenza virus, parainfluenza virus, and human metapneumovirus can also cause bronchiolitis. However, bacteria rarely cause bronchiolitis in children.
The common symptoms of bronchiolitis in children may include
- Runny nose.
- Stuffy nose.
- Fever.
- Wheezing.
- Cough.
- Rapid breathing.
- Vomiting.
- Irritability.
Pulse oximetry, chest X-rays, and blood tests, including arterial gases, can help with the diagnosis. Most treatments are aimed at symptomatic relief, and breathing is monitored during the illness. Breathing troubles require hospitalized care, and antibiotics are usually not required. IV fluids and oxygen supplementation with breathing therapies may be beneficial.
7. Pain
Pain is one of the common problems experienced by most children. Injury, illnesses, and medical procedures can cause acute pain in children and increase stress and anxiety in children and parents. Children can also experience growing pains on the musculoskeletal system, usually in the front of thighs and calves during growth spurts, and they may complain of throbbing or cramping aches. Overindulging in activities can also cause pain and aches in children.
Pain is often inadequately assessed and treated in children. Treatments for pain are aimed at providing symptomatic relief. Acetaminophen (Tylenol) and ibuprofen are usually prescribed for pediatric pains. Although these medications are available over-the-counter, you may talk to the pediatrician for the exact doses based on your child’s weight and age. You may also try warm compresses and massages to relieve pain (8).
Narcotic pain medications are not recommended for children with acute pain due to common injuries and illnesses such as ear pain, leg pain, ankle sprain, or sore throats. Painkillers such as codeine are also not recommended for pediatric use since they may result in life-threatening side effects in children.
8. Common cold

A common cold is an upper respiratory tract infection caused by various viruses. Although many viruses can cause colds in children, rhinoviruses are the most common culprits. These viruses are spread directly from respiratory drops of an infected person while coughing or sneezing or indirectly by touching a contaminated surface or infected person (9).
Most children have six to eight colds per year, and it can be high among younger children attending daycares or child care centers. The incidence may reduce after six years of age. The common symptoms of cold may include
- Runny nose.
- Nasal congestion or stuffy nose.
- Cough.
- Mild fever.
- Muscle aches.
- Watery eyes.
Some children may have green mucus discharge from their noses during viral colds for a few days. Cold symptoms may improve within ten days. To prevent dehydration during a cold, doctors may recommend using humidifiers and ask the child to drink fluids and take enough rest during colds. Some children may receive symptomatic treatments. Antibiotics are only prescribed if bacterial sinusitis is suspected with a common cold.
 Quick fact
Quick fact9. Bacterial sinusitis
Bacterial sinusitis is an inflammation of the lining of the sinus caused by bacteria trapped inside the sinuses. Children can also get viral sinusitis after a common cold and allergic sinusitis related to hay feveriAn allergic reaction to pollen and pet hair causing sneezing, itchy eyes, and coughing (10).
The common symptoms of bacterial sinusitis in children may include
- Cold-like symptoms such as daytime cough and nasal discharge lasting more than ten days.
- Thick yellow nasal discharge and fever for three or more days in a row.
- Irritability.
- Severe headaches.
- swelling around the eyes and light sensitivity.
Antibiotics for ten or more days are prescribed for children with bacterial sinusitis.
10. Cough
A cough is the body’s way of responding to throat or airway irritation. A cough can be dry (without sputum) or wet (productive, with sputum) and of various characteristics depending on the cause. Symptoms of underlying conditions such as fever, nasal congestion or runny nose, and throat irritation, can also be associated with coughs in many cases.
The common causes of cough in children may include
- Viral infections of the airways.
- Bacterial airway infections.
- Cough as a part of normal airway clearance.
- Exposure to cigarette smoke and chemical fumes or gases.
- Improper swallowing of foods.
Cough treatments in children may include the following:
- Antibiotics are prescribed for coughs due to bacterial infections.
- Viral coughs may not require antibiotics, and doctors may recommend use of humidifiers or cool mist vapors.
- You may also try home remedies, such as honey, to relieve cough. However, do not give honey to infants younger than one year since this may cause infant botulismiA condition characterized by muscle weakness and breathing issues caused when babies ingest toxins produced by a specific bacteria .
- Cough syrups and medicines are recommended for children above four to six years. Always seek a prescription for cough medicines since many are not approved for children of a certain age.
Over-the-counter cough medicines can pose serious side effects in babies and children younger than four years (11). Cough medicines containing codeine are not recommended for children under 12 years and children and adolescents up to 18 years with asthma and other respiratory or breathing issues. Codeine is a narcotic cough suppressant, but it can be dangerous since it slows down the heart rate and breathing rate (12).
11. Hand foot and mouth disease
It is one of the most common and contagious viral infections in children (below five years) but may also affect teens and adults. Symptoms include fever, headache, sore throat, and a runny nose, and usually resolve in seven to eight days. A rash of red spots or tiny blisters affects the palms, soles, and the diaper area after a day or two of the fever. The rashes may cause pain but are not itchy.
Treatment includes:
- OTC medications such as acetaminophen or ibuprofen (for children above six months)
- Adequate hydration
- Easy-to-swallow soft foods
- Children above four years can be given throat lozenges and sprays (lidocaine-free)
- Salt-water gargling for children above six years (13).
Children are also vulnerable to many other diseases such as polio, rotavirus, hepatitis, measles, diphtheria, tetanus, pertussis (whooping cough), mumps, and chickenpox. However, childhood immunizations help prevent these diseases. Unvaccinated children have a high risk for vaccine-preventable diseases, especially during outbreaks.
Ways To Prevent Common Childhood Illnesses
Vaccinations as per schedule can prevent many childhood illnesses. You may also consider the annual influenza vaccine (yearly flu shot) for all children above six months of age. This may reduce the incidences and severity of influenza and related complications.
The following home care tips can also prevent common childhood illnesses (14).
- Maintain hand hygiene. Washing hands with soap and water or sanitizing with alcohol-based sanitizer before touching face, nose, or eyes, before eating, after using the toilet, and after coming from outside may reduce the risk of certain viral and bacterial illnesses.
- Follow cough and sneeze etiquette at home. Anyone sneezing or coughing should cover the face and nose with a napkin or elbows to avoid spreading germs in the air.

- Clean high contact areas such as doorknobs, toys, and surfaces with disinfectants
- Avoid exposure to allergic triggers if the child has an allergy.
- Keep children away from infected family members during flu or colds and avoid sharing utensils and personal items.
- Use bathing caps or earplugs to keep the ears dry in children vulnerable to swimmers’ ears.
You may also not let your child go to daycare or childcare centers during any sickness that can be spread to others. Seek a pediatrician’s advice to know the time to return to school or daycare during consultation.
When To See A Doctor
Although many childhood illnesses may resolve without specific treatments, seeking a pediatrician’s advice for exact diagnosis and care is recommended. In addition, any illnesses with severe symptoms and lasting more than usual require medical care.
Sometimes, mild bacterial or viral infections can develop into more serious infections. So you may seek pediatric consultation if the symptoms worsen or worry about new symptoms or complications. You may also inform the doctor if there is no improvement with treatments.
Frequently Asked Questions
1. Why do children fall sick in daycare/school?
Children may catch the flu often in their first few years, especially the first year, of using child care facilities because the flu is one of the most common infections found in these facilities. It is usual for children to suffer from cold, cough, fever, and diarrhea contracted from childcare facilities, but eventually, they can develop immunity against the infections (15).
2. What is the most severe childhood malady?
Pneumonia is considered one of the most severe childhood diseases affecting around 700,000 children per year (16).
3. How can infections spread?
Infections can spread through different means, including (17):
• Aerosol droplets
• Direct contact with an infected person
• Contact with an infected object
• Body fluids
• Environmental spread, such as through food, water, soil, and animals
4. How can I help my child recover from common illnesses?
To support your child’s recovery, make sure they get plenty of rest, eat healthy foods, and drink enough fluids. Also, be sure to follow your doctor’s instructions about any medications or treatments.
All of the above-mentioned common diseases in children are easily treatable and manageable. Most of these pediatric ailments can also be prevented by following the immunization schedule and practicing good hygiene. However, because many of their symptoms overlap, it is best to obtain medical guidance and prescriptions for treatment if your child exhibits any symptoms. Antibiotics should not be given to children without a prescription since many infections are viral. Moreover, with any illness, a nutritious diet, enough fluids, and adequate rest may aid the child’s recovery.
Infographic: Common Diseases In Children
Children tend to be prone to various diseases, including infections, due to their developing immune systems. Learning about these conditions can help you manage the symptoms in your child effectively. The infographic below presents the most common illnesses among children.
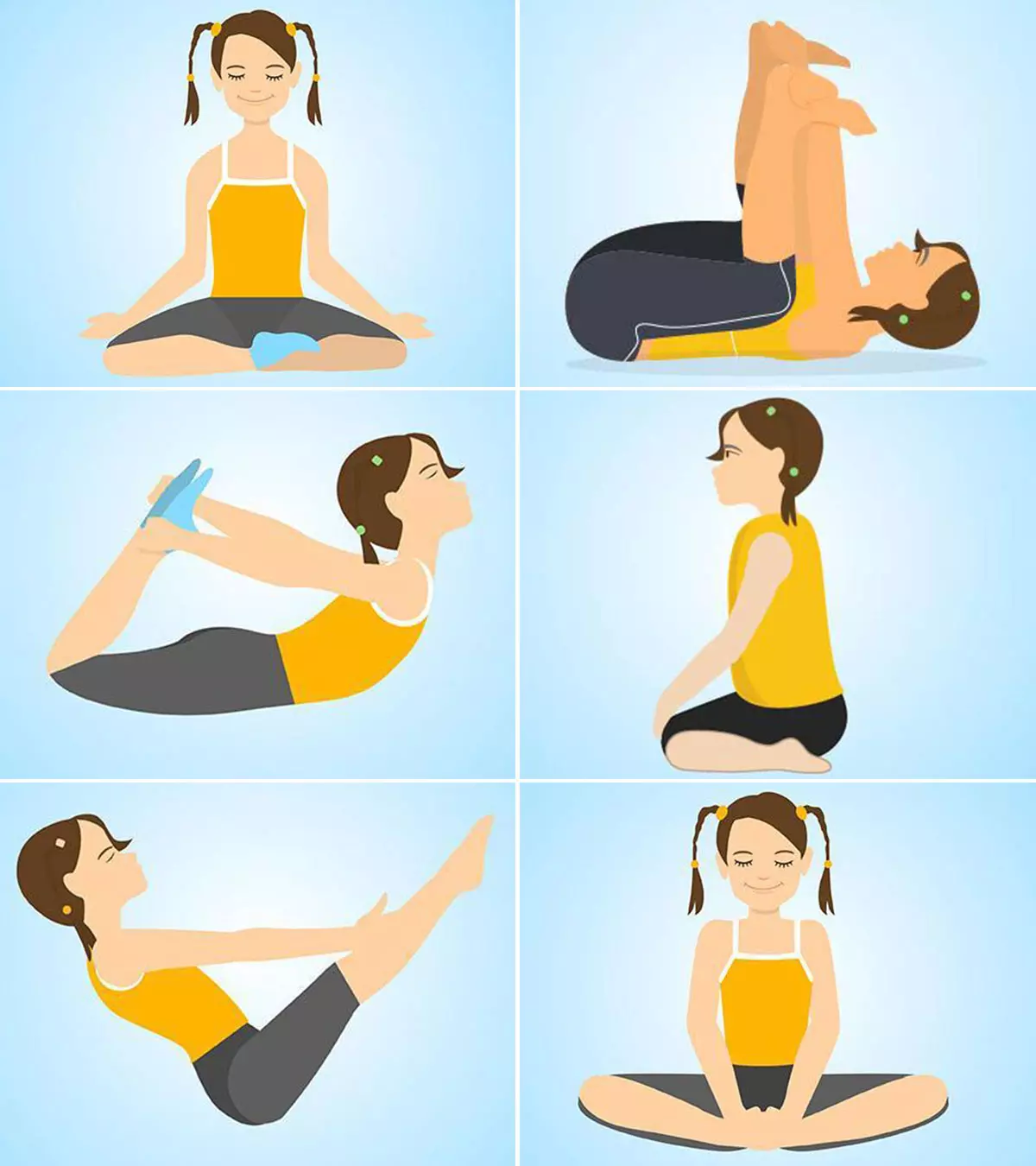
Some thing wrong with infographic shortcode. please verify shortcode syntaxIllustration: Common Childhood Illnesses: Symptoms And Treatment

Image: Dall·E/MomJunction Design Team
With the help of the video below, uncover some signs of childhood ailments like chickenpox, measles, mumps, and whooping cough. Dive into this video to understand their symptoms, treatment, and prevention.
References
- 10 Common Childhood Illnesses and Their Treatments.
https://www.healthychildren.org/English/health-issues/conditions/treatments/Pages/10-Common-Childhood-Illnesses-and-Their-Treatments.aspx - Sore Throat (Viral).
https://www.nationwidechildrens.org/conditions/sore-throat - Ear Pain In Children.
https://www.mottchildren.org/posts/your-child/ear-pain-children - Urinary Tract Infection In Children.
https://www.urologyhealth.org/urology-a-z/u/urinary-tract-infections-in-children - Skin Infections.
https://www.rileychildrens.org/health-info/skin-infections - Acute Bronchitis In Children.
https://www.stanfordchildrens.org/en/topic/default?id=acute-bronchitis-in-children-90-P02930 - Pediatric Bronchiolitis.
https://www.ncbi.nlm.nih.gov/books/NBK519506/ - The Assessment and Management of Acute Pain in Infants, Children, and Adolescents.
https://pediatrics.aappublications.org/content/108/3/793 - Common Cold In Children.
https://www.urmc.rochester.edu/encyclopedia/content.aspx?contenttypeid=90&contentid=P02966 - Sinusitis In Children.
https://www.stanfordchildrens.org/en/topic/default?id=sinusitis-in-children-90-P02063 - Can I give my 5-year-old over-the-counter cough medicine?.
https://www.healthychildren.org/English/tips-tools/ask-the-pediatrician/Pages/Can-I-give-my-5-year-old-cough-medicine.aspx - Codeine not to be used in children below 12 years for cough and cold.
https://www.ema.europa.eu/en/news/codeine-not-be-used-children-below-12-years-cough-cold - Hand-Foot-Mouth Disease.
https://www.nationwidechildrens.org/conditions/hand-foot-mouth-disease - Childhood Illnesses: Six Tips For How To Prevent Them.
https://www.nct.org.uk/baby-toddler/your-babys-health/common-illnesses/childhood-illnesses-six-tips-for-how-prevent-them-archived-archived - When to keep your child home from child care.
https://www.healthychildren.org/English/family-life/work-and-child-care/Pages/when-to-keep-your-child-home-from-child-care.aspx - Childhood diseases.
https://www.unicef.org/health/childhood-diseases#:~:text=HIV%20and%20tuberculosis.- - Ways infectious diseases spread.
https://www.sahealth.sa.gov.au/wps/wcm/connect/public+content/sa+health+internet/conditions/infectious+diseases/ways+infectious+diseases+spread - Urinary tract infection (UTI) in children
https://www.nhsinform.scot/illnesses-and-conditions/kidneys-bladder-and-prostate/urinary-tract-infection-uti-in-children#:~:text=Urinary%20tract%20infections%20(UTIs)%20in - Common Cold in Children
https://www.stanfordchildrens.org/en/topic/default?id=common-cold-in-children-90-P02966
Community Experiences
Join the conversation and become a part of our nurturing community! Share your stories, experiences, and insights to connect with fellow parents.
Read full bio of Dr. Supriya Mahajan
Read full bio of Dr Bisny T. Joseph
Read full bio of Dr. Ritika Shah
Read full bio of Vidya Tadapatri