Image: iStock
The contraction stress test or CST blood test is a method of predicting the baby’s behavior during labor. This test uses artificial contractions to understand how a baby would respond to natural labor contractions by studying their heart rate. This test is mostly performed on high-risk pregnancies. If your doctor has suggested a CST, then here is all you need to know about it. Read on to know more about CST, its method, the risks, and the contradictions in this post.

Key Pointers
- Contraction Stress Test is performed in high-risk pregnancies to predict fetal behavior during labor.
- The method involves studying fetal heart rate during artificial contractions at around 34 weeks of pregnancy.
- Nipple stimulation or low-dose oxytocin may help trigger contractions during the study.
- A normal/negative result is indicated if no fetal heart rate deceleration is recorded at the rate of 3 contractions/10 minutes.
- The test cannot be performed on women carrying multiples as it is contraindicated.
What Is A Contraction Stress Test (CST)?
CST measures the fetal heart rate during late pregnancy or labor. The purpose of this test is to induce contractions and ensure that the baby is getting sufficient supply of oxygen from the placenta during uterine contractions. This test is also known as the Stress test or the Oxytocin challenge test.
Women with pregnancy complications are generally subjected to this test at around 34 weeks or later (1). Moreover, the number of tests a pregnant woman may need depends upon the extent of risk in her pregnancy.
CST is recommended if the doctor thinks your pregnancy poses risks, especially to the baby.
Why Is CST Done?
CST is done to determine the fetal well-being during contractions or labor and to check if the placenta is adequately supporting the fetus. If the placenta has enough oxygen and blood for the fetus, then the heartbeat will not be affected.
The average fetal heart rate is 110-160 beats/minute and can fluctuate based on the uterine conditions. Any abnormality in the fetal heart rate indicates an insufficient supply of oxygen or some other fetal distress (2). Usually, the uterine contractions decrease the flow of blood or oxygen to the fetus through the placenta. This could bring a variation in the fetal heart rate.
The contraction stress test is recommended when the results of a non-stress test or biophysical profileiTest done after the 28th week of pregnancy to evaluate the fetal health through imaging and monitoring of fetal heartbeat. are abnormal (1).
A contractions stress test is needed especially in high-risk pregnancies with complications such as (3), (4):
- Heart disease
- Type-1 diabetes
- Rh-factor sensitizationiThe phenomenon when a mother’s Rh-negative blood mixes with a baby’s Rh-positive blood to create maternal antibodies.
- Poorly controlled hyperthyroidismiA condition marked by excess thyroid hormones in the body, leading to weight loss, increased heart rate, and other symptoms.
- Antiphospholipid syndromeiA condition in which the immune system mistakenly attacks tissues of the body by forming blood clots.
- Systemic lupus erythematosusiAn autoimmune, inflammatory disease in which the immune system attacks its tissues.
- Hypertensive disorders
- HemoglobinopathiesiA group of inherited disorders in which there is an abnormal number or structure of the hemoglobin molecule. such as hemoglobin SiA mild form of sickle-cell anemia, where hemoglobin S and C genes are inherited from both parents, that affect the red blood cells. gene causes the red blood cells to become sickle-shaped, SC or S-thalassemiaiAn inherited blood disorder that reduces hemoglobin levels and causes the red blood cells to become sickle-shaped and brittle.
- Chronic renal disease
- Intrauterine growth restriction
- High BP

- Post-term pregnancy
- Stillbirth
- Decreased fetal movements
- Multiple (twin or triplet) pregnancy with growth discrepancy
- Oligohydramnios, or deficiency of amniotic fluid
- Polyhydramnios, or excess amniotic fluid
The following section details how the test is carried out at the hospital.
How Is The Contraction Stress Test Done?
Before the test, you are told not to eat or drink anything for six to eight hours. Also, the patient needs to empty her bladder before the procedure starts.
 Point to consider
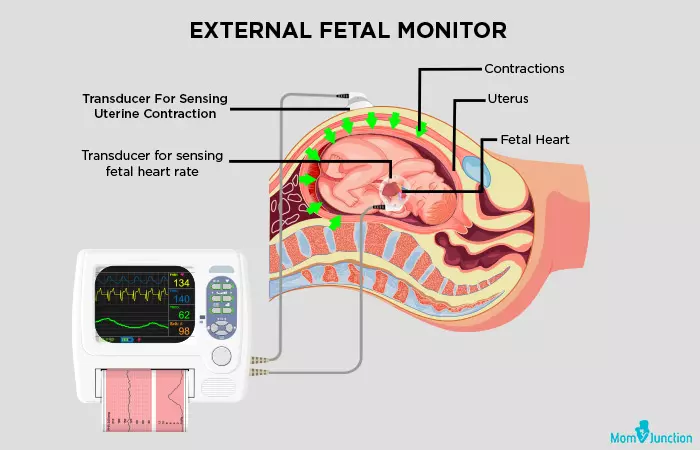
Point to considerThe test: You have to lie to your left side, and two devices are strapped around your belly. One device monitors the fetal heartbeat and the other records the uterine contractions. The heartbeat and the contractions are recorded on a graph paper to evaluate the result.

The test lasts until you get three contractions (each lasting for 40 seconds) within ten minutes (5). The contractions that you feel may be mild, similar to menstrual cramps.
- Oxytocin challenge test: If the contractions do not start on their own within 15 minutes, then a small dose of oxytocin (Pitocin) is given to you through IV.
- Nipple stimulation: It is another method to kick-start the contractions. The doctor may ask you to stimulate the nipples to release oxytocin in the body and trigger contractions naturally.
After the test, you need to wait until the contraction frequency gets back to normal. So the overall time taken for the test is around two hours.
How Does It Feel During The Contraction Stress Test?
Lying on your left side may not be comfortable for you during the contractions. Moreover, the electronic sensors around your belly may make you feel a bit uncomfortable. Most women who have undergone this test have said that it is a painless but uncomfortable procedure (1).
Keep reading to know how the doctors interpret the CST results.
How Is The CST Result Interpreted?
The contraction stress test results are obtained immediately from the graphical record in the electronic device used for fetal monitoring during the test (4). Results could be:
- Negative contraction stress test
The CST result is normal/negative when there are no decelerations in the fetal heart during the contractions, recorded at the rate of 3 contractions/10 minutes.
- Positive contraction stress test

The test result is positive if more than half of the contractions indicate late decelerations in the fetal heart rate, recorded at the rate of 3 contractions/10 minutes.
- Equivocal-suspicious
 Quick fact
Quick factIntermittent decelerations or a significant variance in the decelerations is noticed. This ambiguity calls for a repeat test.
- Equivocal-tachysystole
There is one contraction in more than every two minutes, which lasts for 90 seconds, indicating fetal heart rate decelerations.
- Equivocal-unsatisfactory
The result is unsatisfactory when fewer than three contractions occur in 10 minutes or when the tracing cannot be interpreted properly.
Heather, a mom and blogger, recounts how she had a C-section after a positive CST test. She shares, “I’m hooked up to pitocin(oxytocin), starting with a small dose that is increased every 20 minutes. Barbara, the nurse, is awesome. She monitors every blip on the monitor. Things are looking good at the start of the test. I am certain that we will have at least another week of pregnancy.
“Jackson’s (the baby) heart rate looks great through each contraction until I’m at the highest dose of pitocin. His heart rate starts to slow down at the end of each contraction. So it’s a call to Doc again…Jackson’s heart rate is decelerating at the end of each strong contraction. This indicates that he will not handle labor well. His blood flow/oxygen flow could be compromised. Which could mean brain damage from labor. His (doctor’s) strong suggestion to us is to opt for a c-section (i).”
If you find yourself in a similar situation, it’s crucial to consider the medical advice given and make the best decision for the health of the mother and the baby.
Like a few other tests, this test may also have some risks.
What Are The Risks Of This Procedure?
Some of the risks of CST are: (1):
- The use of oxytocin could lead to early labor. It may also prolong the contractions, but they can be stopped with the help of medicines. If the contractions do not subside, an emergency delivery will be recommended by the doctor.
- The fetal heart rate monitoring device may be faulty and indicate health problems in your baby even though the baby is doing good.
- False positive contraction stress test could happen when the contraction stress test shows a drop in the fetal heartbeat when your baby is healthy. The test result could also be falsely positive in the case of patients with hypertension.
Though the test is done in the case of high-risk pregnancies, it is not recommended for a certain group of pregnant women.
What Are The Contraindications For This Test?
Contraction stress test might not be viable in some cases.
- Women carrying multiples, because this test could stimulate preterm labor.
- A patient with a ruptured membrane from a previous pregnancy or uterine surgeries.
- Any signs of preterm labor.
- Patient with a previous classical c-section.

- Obesity.
- Placenta abruption or placenta previaiA pregnancy complication where the placenta obstructs the cervix, causing difficulties in vaginal delivery. .
- Patient with an incompetent cervix.
- Gestation age is less than 32 weeks.
- If the baby’s movements are more during the test, it becomes difficult for the device to record the heartbeat or contractions.
Next, we understand how the contraction stress test is different from the non-stress test.
CST Vs. NST
Here are the differences between the non-stress test (NST) and contraction stress test (CST) (6):
| CST | NST |
|---|---|
| The fetal heart rate is recorded in response to the uterine contractions. | Fetal heart rate is measured in response to fetal movement, without putting any stress on the fetus. |
| Nipple stimulation or oxytocin is used to start a uterine contraction. | Uterine contractions are not triggered in this procedure. |
| The test results are read as negative (normal) or positive (abnormal). | The test results are read as reactive (normal) or non-reactive (abnormal). |
| It is expensive and cumbersome. | It is cost-effective, quick, and safer. |
| Not commonly used nowadays. | Preferably recommended by doctors nowadays. |
 Quick fact
Quick factFrequently Asked Questions
1. What happens if a baby fails a stress test?
“Failing” a contraction stress test corresponds to getting a positive result on the test. In such a case, late decelerations in heart rate (slowed heart rate) are observed in more than half of the contractions (4). It may indicate insufficient oxygen supply or other complications.
2. Does everyone require a non-stress test during pregnancy?
Not all pregnant women require a non-stress test. It is suggested in case of underlying chronic health issues, a history of complicated pregnancies, multiple pregnancies, slow fetal movements, and other indicators of probable pregnancy complications (6).
3. Do Braxton Hicks show on NST?
No, laboratory or radiographic tests cannot diagnose Braxton Hicks contractions. These contractions are evaluated by assessing the pregnant woman’s abdomen, specifically by palpating the contractions (7).
4. Can I eat before a non-stress test in pregnancy?
Yes. In fact, doctors may suggest you eat something before the test since babies usually show increased movement after their mothers have eaten (8).
5. Can a contraction stress test be done at home?
No, a contraction stress test cannot be performed at home as it requires specialized medical equipment and trained personnel.
6. How often should a contraction stress test be done?
Contraction stress tests assess the baby’s health and may be done several times in the last weeks of pregnancy. If the test turns out positive, it indicates that the baby may be unable to tolerate labor contractions. In such cases, the test may be scheduled again a few weeks later (10).

CST test during pregnancy helps determine if the baby is getting sufficient blood and oxygen during contractions. This test is advised around 34 weeks of pregnancy if you have abnormal non-stress test results. It is also recommended for women with pregnancy complications such as heart disease and type-1 diabetes. The CST test can be safely used in most cases. However, it isn’t viable if the expecting mother has placental abruption or placenta pervia, incompetent cervix, or a gestational age of lesser than 32 weeks.
Infographic: Key Contraindications For Contraction Stress Test
During a high-risk pregnancy, your doctor may recommend a contraction stress test at the 34th week of pregnancy to check the fetus’ well-being by stimulating contraction. However, even if you’re in a high-risk pregnancy, there are conditions where this test might not give viable results. Check out the infographic below to learn about such conditions during pregnancy.
Some thing wrong with infographic shortcode. please verify shortcode syntaxIf you have a high-risk pregnancy, your doctor may recommend a contraction stress test during late pregnancy to monitor fetal heart rate. Look through this video to learn more about this test and how is it done.
Personal Experience: Source
MomJunction articles include first-hand experiences to provide you with better insights through real-life narratives. Here are the sources of personal accounts referenced in this article.
i. Jackson Jerry Turner.https://hmft.blogspot.com/2006/12/jackson-jerry-turner.htmlReferences
- Contraction Stress Test.
https://my.clevelandclinic.org/health/diagnostics/22849-contraction-stress-test - Non-stress/contraction Stress Tests (fetal heart rate testing).
https://www.uclahealth.org/medical-services/obgyn/maternal-fetal-medicine/diagnostic-tests-and-procedures/non-stresscontraction-stress-tests-fetal-heart-rate-testing - Monica Preboth; ACOG Guidelines on Antepartum Fetal Surveillance; American Academy of Family Physicians (2000).
https://www.aafp.org/pubs/afp/issues/2000/0901/p1184.html - Contraction Stress Test.
http://www.hhma.org/healthadvisor/aha-strstst-wha/ - Lawrence D. Devoe MD; Nonstress and Contraction Stress Testing; The Global Library of Women’s Medicine.
https://www.glowm.com/section-view/heading/Nonstress%20and%20Contraction%20Stress%20Testing/item/210# - Nonstress Test.
https://medlineplus.gov/lab-tests/nonstress-test/ - Deborah A. Raines and Danielle B. Cooper; (2025); Braxton Hicks Contractions.
https://www.ncbi.nlm.nih.gov/books/NBK470546/ - Nonstress Test.
https://www.hopkinsmedicine.org/gynecology-obstetrics/specialty-areas - M W Keane et al.; (1981); Comparative study of stressed and nonstressed antepartum fetal heart rate testing.
https://pubmed.ncbi.nlm.nih.gov/7465146/ - Contraction Stress Test
https://my.clevelandclinic.org/health/diagnostics/22849-contraction-stress-test
Community Experiences
Join the conversation and become a part of our nurturing community! Share your stories, experiences, and insights to connect with fellow parents.
Read full bio of Dr. Asmita Kaundal
Read full bio of shreeja pillai
Read full bio of Rebecca Malachi
Read full bio of Dr. Joyani Das