Image: Shutterstock
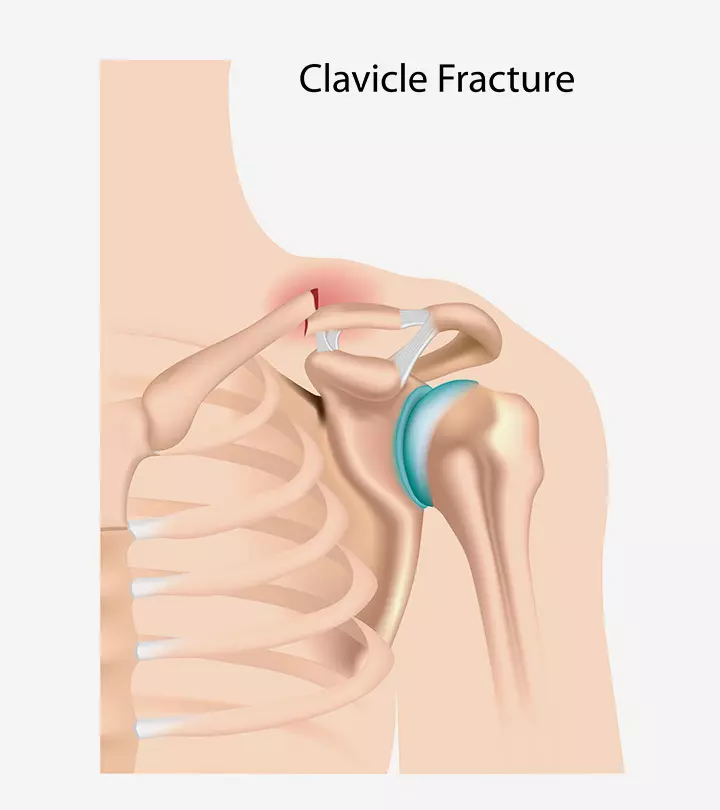
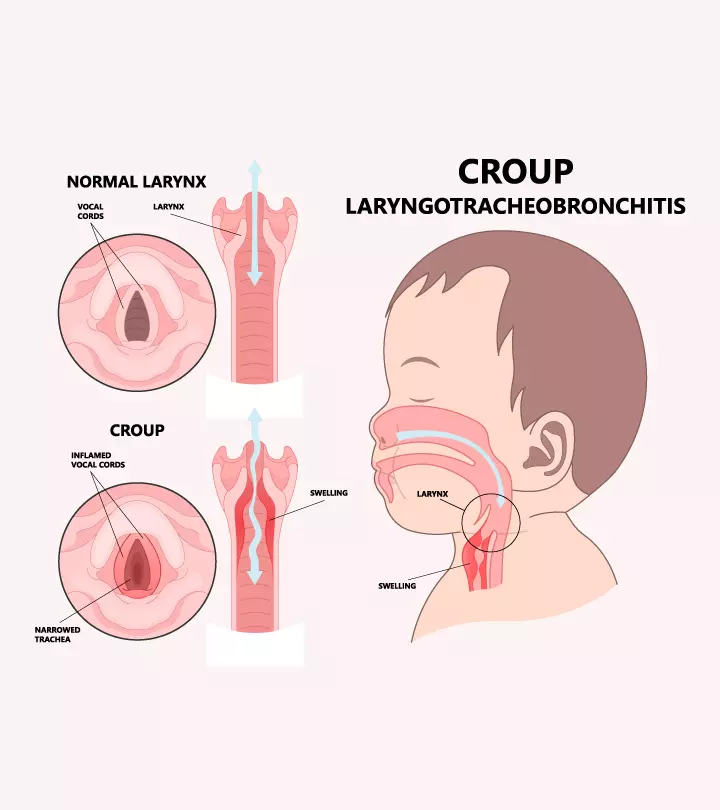
Croup in kids occurs due to a viral infection in the vocal cords and the trachea (windpipe). The infection causes swelling and narrowing of the upper airway, making it difficult for air to pass through. It is characterized by a harsh, barking cough, hoarseness, and high-pitched noise while breathing in (1).

Croup infection usually affects young children, and the symptoms are generally mild and can be treated at home. However, severe and prolonged croup infections may cause breathing difficulty and warrant hospitalization (1) (2).
Read on to learn about the causes, symptoms, risk factors, and treatment options for croup in children.
Key Pointers
- Croup is a viral infection, causing respiratory distress in children.
- Intense coughing, rapid and troubled breathing, fatigue, and rough voice are characteristic signs of this infection.
- This condition is treatable with oral medications (corticosteroids) and nebulization.
- Scroll down to know when to contact your child’s healthcare provider.
What Causes Croup In Children?
Croup is commonly caused by the human parainfluenza virusiCauses upper and lower respiratory infections in children and adults, such as colds, pneumonia, and bronchitis. (types 1 and 3). However, influenza A and B viruses, respiratory syncytial virusiMostly causes mild respiratory infections such as the common cold in otherwise healthy children. , rhinovirus, coronavirus, human metapneumovirusiCauses upper and lower respiratory infections in children, older adults, and those with weak immune systems , and adenovirus may also cause croup infection.
Viral croup is the second most common cause of respiratory distress in children below ten years, and the viral infection in children affects boys more than girls (3).
Symptoms Of Croup In Children
Croup generally begins with cold-like symptoms, such as a runny nose, fever, and cough. The following symptoms are observed after 24–72 hours of the respiratory infection. The symptoms seem to worsen during the night and fluctuate, depending on whether the child is calm or agitated (1) (3).
The main symptoms include:
- Harsh coughing, which often sounds like barking
- Noisy breathing with a high-pitched, squeaky sound, known as stridor
The symptoms can be categorized based on the level of severity.
Mild infection
- Occasional barky cough
- Stridor while sleeping or not present at all
- Mild indrawing of area above neck called supraclavicular area
Moderate infection
- Frequent barky cough
- Easily audible stridor during sleep
- Limited or no distress
- Visible indrawing of supraclavicular area
Severe
- Frequent barky cough
- Prominent stridor during inhalation and occasional stridor while exhaling
- Noticeable distress or agitation
- Lethargy
- Severe indrawing of supraclavicular area
- Can lead to complete airway obstruction which can cause difficulty breathing and even failure of breathing, if not treated in time Severe indrawing of supraclavicular area
- Can lead to complete obstruction of airways and failure of breathing, if not treated in time, thus leading to a pediatric emergency.

Other symptoms include
- Flu-like symptoms such as sneezing and a runny nose
- Fever
- Hoarse voice
- Red eyes
- Poor appetite
The symptoms are short-lived. Approximately 60% of children experience a reduction of barky cough by 48 hours or less, and only in about less than 2% of children, the cough might persist for more than five nights (3).
Who Are At Risk Of Contracting Croup?
The risk of contracting croup infection increases based on the age of the child and specific seasons. It is commonly seen in children between six months and three years. However, it can occur in children up to six years of age. Croup infections occur in a predictable pattern, with the infections seen in late fall and winter.
Recurrent croup infections (more than two episodes per year) are found in children who
- Had prior intubationsiThe process of making a person breathe by passing an endotracheal tube into the patient's airway through the nose or mouth. .
- Are premature.
- Are younger than three years.
Gastroesophageal reflux disease (GERD) and asthma are commonly found in patients with recurrent croups, but these may not increase the risk (4).
 Quick fact
Quick factIs Croup Contagious?

Yes, croup can spread from one child to another through respiratory droplets when children with croup cough or sneeze. It also spreads when a healthy child touches their face, nose, or eyes after coming into contact with contaminated surfaces, such as doorknobs.
Physical examination and pediatric history are the two diagnostic methods to detect croup in children. In some rare cases, such as when the child is asymptomatic or when the diagnosis is unclear, the doctor might recommend radiography or laryngoscopyiAn examination of the back of the throat and the voice box using a tube called a laryngoscope. (3) (4).
 Quick fact
Quick factTreatment For Croup In Children
Mild to moderate croup infection can be treated at home with oral corticosteroidsiDrugs that may help reduce inflammation. and nebulized epinephrineiA neurotransmitter and a hormone used to treat severe allergic reactions .
Severe cases require hospitalization. These medications help in minimizing the symptoms by reducing the inflammation in the child’s airway. The cough in babies may not reduce, but stridor and inward drawing of chest walls may subside (4).
When your child experiences no stridor or chest wall indrawing at rest, they may go home (if the child is hospitalized). However, your doctor is the best person to estimate your child’s condition.
J. R. Heimbigner, a father to three and an author, shares the symptoms his daughter experienced with croup, “The previous night, our little girl woke up with a Croup cough. She has had a rough cough and breathing before, so we had done everything we normally do and got her back to bed. Normally, she wakes up in the morning better. Sunday morning, she sounded just as bad. The day progressed, and she wasn’t improving, it was time to go to urgent care. As they headed out the door, I assumed they’d be back in no time at all. I never imagined I would get a call from my wife saying the breathing treatment worsened my daughter’s condition. We discussed our next steps objectively and went from there. My daughter was transported by ambulance to the hospital, where she received additional breathing treatment. My daughter was discharged the next day (i).”
 Point to consider
Point to considerHome-Care Tips For Croup In Children
If your child has a mild infection, you may follow the below home-care tips to relieve the symptoms (3).
- Try not to agitate or upset your child, as distress can worsen the stridor and other symptoms.
- If your child is crying, place them on your lap in a comfortable position.
- Give them fluids to soothe their sore throat.

RSV vs. Croup
Respiratory Syncytial virus (RSV) causes a viral infection in babies and children, producing symptoms resembling the common cold. It may or may not result in croup. Croup, though majorly caused by viral respiratory infections, may have other types caused due to an allergy or reflux from the stomach (spasmodic croup) (5).
An RSV vaccine between 32 through 36 weeks of pregnancy may protect newborns. High-risk babies aged 8 to 9 months may be eligible to receive the RSV vaccine named palivizumab. However, there is no such particular vaccine for croup (6).
Whooping Cough vs. croup
Whooping cough, a symptom of pertussis, is characterized by a “whooping” or “hoop” sound that occurs when deep inhalation is attempted after a round of several coughs in a row. Whereas, croup produces a distinctive barking cough. Whooping cough occurs due to a bacterial infection (child may be protected via the diphtheria/tetanus/pertussis or DTaP vaccination), whereas the majority of croup episodes are due to a viral infection (7) (8).
When To See The Doctor?
If you find any of the below symptoms in your child, you need to visit your child’s doctor (1) (2).
- Fatigue or lethargy
- Decreased levels of consciousness
- Trouble breathing
- Body turning blue or pale due to lack of oxygen
- Sudden high temperature
- Difficulty swallowing
- Inability to speak
Prevention Of Croup
You can protect your child from croup infection or prevent your child from infecting someone by taking the following precautions.
- Make sure they wash their hands before eating and after coming home from school or the playground.
- Instruct them not to touch their face, nose, or eyes before washing hands.
- If someone has a croup, ask your child to maintain physical distance until they get well.
- Keep your child’s vaccinations up to date.
- Give them nutritious foods that can help boost their immunity.
- Encourage them to cover their nose and mouth while coughing and sneezing.

Adults may rarely get infected. However, it is best to be careful while taking care of your child. As the infection is contagious, do not send your child to school until the symptoms subside or for at least three days.
Frequently Asked Questions
1. How long is a child with croup contagious?
People with croup virus may be contagious for three to 16 days (9). You may not notice the symptoms in the initial two to three days, but you will eventually.
2. Does the croup go away on its own?
Yes, a child with a croup infection may feel better within 48 hours without any medical intervention (2). But if your child is suffering, it is better to consult a doctor.
3. Is croup more common in boys or girls?
About 3% of children are affected by croup in the US every year, and the occurrence of croup is slightly more in boys than girls (10).
4. What is the difference between croup and bronchiolitis in children?
Croup is an acute illness of the respiratory system that is characterized by hoarseness in the voice, a barking cough, and inspiratory stridor. On the other hand, bronchiolitis is a viral infection of the bronchioles that is associated with symptoms such as cough, mild fever, and coryza (11) (12).
5. Is there a vaccine available to prevent croup in children?
Currently, there is no specific vaccine available to prevent croup. However, proper administration of certain vaccinations, including measles, diphtheria, and Haemophilus influenzae type b (Hib) during childhood, can help in reducing the risks of croup in children (10).
Croup in kids is a contagious viral infection that affects the respiratory system. Mild to moderate croup infection can be treated at home, whereas severe infection warrants hospitalization. In most cases, croup abates in one to two weeks. Taking ample rest and drinking plenty of fluids are simple home remedies that could provide symptomatic relief and hasten recovery. Consult a doctor promptly if the child has additional symptoms, such as troubled breathing. Maintaining proper hygiene and keeping a child’s vaccinations up to date are effective measures to prevent the infection.
Infographic: How To Manage And Prevent Croup In Children?
Younger children are more prone to croup, a viral infection characterized by a hoarse voice, barky cough, and noisy breathing. The treatment depends on the severity of the condition. But, home care management plays an important role in quicker recovery. Explore the following infographic for various homecare and prevention tips for croup in children.
Some thing wrong with infographic shortcode. please verify shortcode syntaxIllustration: Croup In Children: Symptoms Causes Risks And Treatment

Image: Dall·E/MomJunction Design Team
Croup is a common childhood illness, but it can be scary. Learn more about croup in children through this video.
Personal Experience: Source
MomJunction articles include first-hand experiences to provide you with better insights through real-life narratives. Here are the sources of personal accounts referenced in this article.
i. A night at the children’s hospital;https://jackheimbigner.medium.com/a-night-at-the-childrens-hospital-6a6227069ecc
References
1. Croup; The Royal Children’s Hospital Melbourne
2. Croup; NHS
3. Candice L. Bjornson and David W. Johnson; Croup in children; CMAJ (2013).
4. Dustin K. Smith, Andrew J. McDermott, and John F. Sullivan; Croup: Diagnosis and Management; American Family Physician (2018).
5. Croup and your young child; American Academy of Pediatrics
6. RSV: When It’s More Than Just a Cold; American Academy of Pediatrics
7. Croup; Cleveland Clinic
8. Cough; Boston Children’s Hospital
9. Parainfluenza; Parainfluenza
10. Croup; Yale Medicine
11. Croup or bronchiolitis; Department of Health, Victoria
12. Bronchiolitis; Cleveland Clinic
13. Croup in Children; Cedar’s Sinai
Community Experiences
Join the conversation and become a part of our nurturing community! Share your stories, experiences, and insights to connect with fellow parents.
Read full bio of Dr. Anuradha Bansal
Read full bio of Dr Bisny T. Joseph
Read full bio of Dr. Ritika Shah
Read full bio of Shinta Liz Sunny