Image: Shutterstock

The endometrium thickness in pregnancy plays an essential role in determining issues during pregnancy. The endometrium is the uterine lining where the embryo implants to commence pregnancy.
The endometrium’s thickness changes in each pregnancy month, and it is also a parameter assessed during imaging tests (ultrasound scans). The obstetrician may check the endometrium thickness to determine the underlying cause of any abnormal uterine bleeding during pregnancy. Keeping track of endometrial thickness is essential, as it can reveal early signs of issues, enabling timely interventions that help safeguard the health of both the mother and the baby.
In this post, we tell you about the normal endometrium thickness during pregnancy and the various abnormal changes in the tissue’s thickness.
Key Pointers
- The thickness of the endometrial lining changes during ovulation to allow the fertilized egg to implant.
- Depending on the stage of the menstrual cycle, the typical thickness of the endometrium varies.
- Endometrial disorders such as cancer can produce thickened endometrium in non-pregnant women.
- Menopause is the most prevalent and natural cause of endometrium thinning.
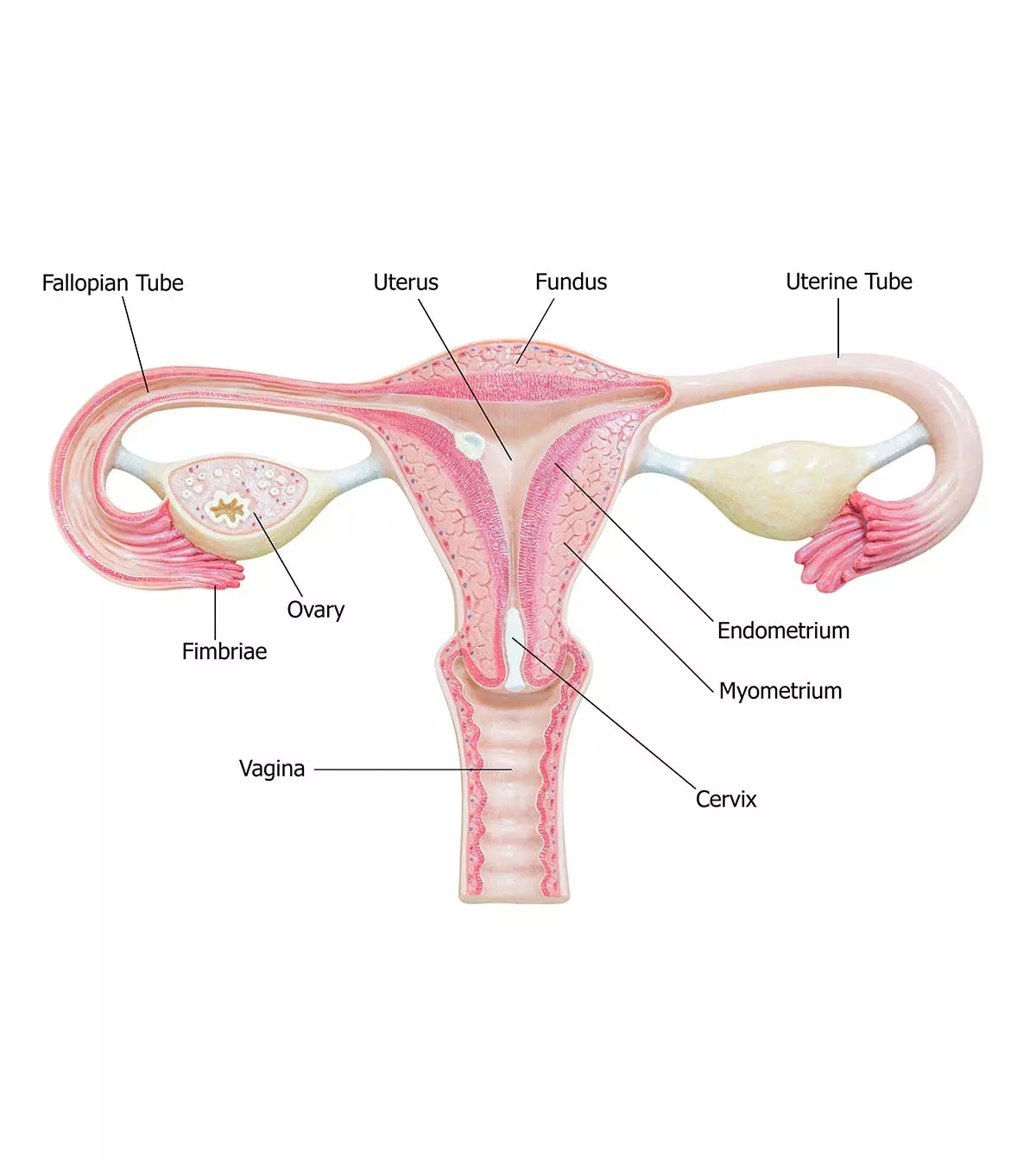
What Is The Endometrium?
The endometrium is a vital part of the reproductive system. It is the inner lining of the uterus, where implantation of the embryo takes place. It comprises a single-layered prismatic epithelium and cell-rich connective tissue with blood vessels that surround the uterine glands. The single-layered prismatic epithelium consists of three types of cells: secretory cellsiCells commonly found in the digestive and respiratory tract that are responsible for producing and secreting molecules. , cells with ciliaiHair-like projections involved in signaling pathways for the regulation of cell growth, differentiation, and migration. , and basal cellsiPart of the innermost layer of the epidermis involved in the creation of new cells. .
The endometrium undergoes various morphological and functional changes during menarcheiThe time when a woman experiences her first period. . As the level of sex hormones changes in the body during ovulation, the thickness of the endometrial lining also changes to enable the implantation of the fertilized egg. If fertilization doesn’t happen, then the endometrium lining (functional layer) sheds, leading to menstrual flow (1).
Note: The morphology and thickness of the endometrium remain constant before puberty and in menopause.
Normal Thickness Of The Endometrium
The normal thickness of endometrium varies at different stages of the menstrual cycle in premenopausal women.
The normal endometrial thickness measurements are (2):
| STAGES | THICKNESS |
|---|---|
| During menstruation | 2 – 4mm |
| Early proliferative phase (day: 6-14) | 5 – 7mm |
| Late proliferative/Preovulatory phase | Up to 11mm |
| Secretory phase (ovulation) | Up to 16mm |
According to a study conducted in Shanghai Jiaotong University, the rate of implantation, clinical pregnancy, and ongoing pregnancy was higher among women who had an endometrial thickness between 8-14mm. The pregnancy rate was negatively affected among the women with stripe’s thickness less than 7mm (3).
Endometrial thickness can also be used as a predictor for normal intrauterine pregnancy if there is vaginal bleeding and sonographic diagnosis of pregnancy of unknown location, or other pregnancy complications. (4).
The following chart can give you a better idea of how the thickness of endometrium varies during the cycle.
 Point to consider
Point to consider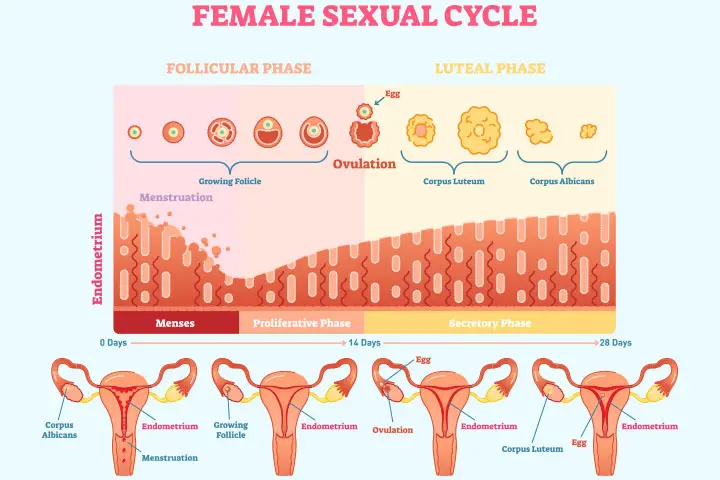
What Causes Thickness of Endometrium?
Both pregnant and non-pregnant women can have an abnormally thickened endometrium due to various reasons (5).
A moderate increase in endometrial thickness for a pregnancy could indicate:
- mola, which can make the endometrium look thick
- Pseudogestational sac
- Retained products of conception
- Heterogeneously thickened endometrium, which could be due to fluid collection
- Heterogeneously thickened endometrium due to an intrauterine blood clot
- Molar pregnancy, wherein the multiple small cystic spaces make the endometrium look thickened
- Inflammation of the uterus, also called endometritis
In non-pregnant women, it could be because of:
- Endometrial carcinoma that gives it a thickened appearance
- Endometrial hyperplasia or over-thickening of the endometrium
- Endometrial polyp, or benign protrusions on the endometrial surface
- TamoxifeniA drug used to treatment of cancer and prevent its recurrence. -related changes causing variable appearances of the endometrial surface
- Endometritis
 Did you know?
Did you know?What Are The Symptoms Of An Abnormally Thick Endometrium?

Image: Shutterstock
The symptoms of an abnormally thick endometrium lining, also known as endometrial hyperplasia, include (6):
- Heavier bleeding during periods
- Longer periods than usual
- Menstrual cycle shorter than 21 days or longer than 38 days
- Spotting between periods
It is recommended that you visit your doctor who specializes in gynecology, if you are experiencing abnormal vaginal bleeding and pelvic pain.
How Is Abnormally Thick Endometrium Diagnosed?

Image: Shutterstock
Transvaginal ultrasound helps in identifying abnormal endometrium thickness (7).
According to obstetrician and gynecologist Dr. Nandita Palshetkar, “Endometrial thickness measurements can be affected by various factors such as the specific ultrasound technique used and the woman’s menstrual cycle. A qualified healthcare professional interprets the measurements in conjunction with the patient’s medical history and overall clinical picture.”
What Does The Endometrium Look Like?
The endometrium looks like a dark line on an MRI or ultrasound scan, and it is called endometrial stripe. Here is how the appearance and thickness of endometrial stripe change during the menstrual cycle (2):
- Menstrual and early proliferative phase: In this phase, it appears as a thin and bright echogenic stripeiRelated to the endometrium when it appears as a dark line during an MRI or an ultrasound. that consists of a basal layer with minimal fluid.
- Late proliferative phase: A trilaminariRelated to something that appears to have a triple layer or lines. appearance is seen in this phase. It comprises the basal layer, middle functional layer, and the inner echogenic stripe at the center.
- Secretory phase: Endometrium is the thickest during this phase. The stripe has fluid surrounding it and thus looks uniformly echogenic in an ultrasound.
How Is It Treated?
You should see the doctor and discuss the treatment options. Treatment will depend on the cause for thickening (6).
What Causes Thinning Of The Endometrium?

Image: Shutterstock
Thin endometrium results from the impairment of the normal growth of the endometrial tissues. The most common cause is menopause and it is natural. (8):
Other causes are (6):
- Permanent damage to the basal endometrium
- The resistance of estrogen by endometrium surface receptors
- Decreased blood flow to the endometrium
- Testosterone overexposure
Can Endometrial Thickness Indicate Early Pregnancy?
Endometrial thickness can indicate early pregnancy, be it normal or abnormal (ectopic). According to research reports from the University of Texas Southwestern Medical Center, Endometrial thickness between 8-40mm was noted in intrauterine pregnancies of unknown location. Among this, 70% of women had an endometrial thickness between 13-25mm. This study also shows that 70% of women with ectopic gestation had an endometrial thickness of less than 13mm (9).
An anonymous mother and a blogger share her experience of getting misdiagnosed with cysts on breasts and endometrium thickness, which later turned out to be a pregnancy. She writes, “I have had a few cysts on both breasts and stomach and also endometrium thickness when I did a check-up at a clinic… The pain has caused me so much, especially in my stomach area; it was like a very heavy stomach twist up so hard that it hit me… My period has not come up since too.. almost close to 2 months. I was a little worried.
“Doctor then examined me on ultrasound and told me it was a baby… I said wait, I had cysts and endometrial thickness. She checked on my tummy again. She said there was no cyst and endometrium thickness at all! What she has checked is a baby (i)!”
[Read: Do Ovary Cysts Affect Pregnancy?]
Frequently Asked Questions
1. Does an endometrial thickness of 17mm mean pregnancy?
Having an endometrial thickness of 17mm before pregnancy means you have a good chance of conception and a better clinical outcome, which is an essential part of reproductive health (10).
2. Does the endometrium thicken after implantation?
Yes. After embryonic implantation, the thickened endometrium from the proliferative phase of the menstrual cycle thickens. It serves as a site for an embryo’s attachment and nourishment during its first few weeks (11).
3. Can I get pregnant with an 8mm endometrium?
Normal endometrial thickness for pregnancy is between 8–14mm, which is ideal for conception. But, it is possible to become pregnant with a lining less than 7–8mm thick. However, your pregnancy rate may be lower (11).
The endometrium is a crucial tissue in a woman’s body that holds the key to a successful and healthy pregnancy. Therefore endometrial thickness in pregnancy helps doctors determine the progress and state of the pregnancy, including any abnormalities and the progress of the pregnancy, which is crucial for ensuring optimal maternal health and fertility. Therefore, awareness about the signs of changing or unusual endometrium thickness is essential as it may indicate an underlying issue such as molar pregnancy, blood clots, or endometritis. Consult your doctor in case of any such abnormal symptoms to seek timely treatment and prevent any complications.
Infographic : How To Improve Endometrium Function And Thickness Before Pregnancy?
Reaching ideal endometrial thickness and functions before conception increases the chance of pregnancy. It also enhances the outcomes of assisted reproductive technologies. Go through the infographic to learn ways to enhance endometrial functions and thickness before pregnancy.
Some thing wrong with infographic shortcode. please verify shortcode syntax
Have you any experiences to share? Please share them in the comments section below.
Personal Experience: Source
MomJunction articles include first-hand experiences to provide you with better insights through real-life narratives. Here are the sources of personal accounts referenced in this article.
i. It is a child blessing;https://sweetrainfall.blogspot.com/2017/03/it-is-child-blessing.html
References
1. The Menstrual Cycle: An Overview; Stanford Children’s Health.
2. Dr Henry Knipe, Dr Yuranga Weerakkody, et al.; Endometrial thickness
3. Yu Wu, et al.; Endometrial thickness affects the outcome of in vitro fertilization and embryo transfer in normal responders after GnRH antagonist administration
4. Moschos E, Twickler DM; Endometrial thickness predicts intrauterine pregnancy in patients with pregnancy of unknown location; NCBI (2008)
5. Dr. Daniel J Bell and Radswiki et al.; Abnormally thickened endometrium (differential); Radiopaedia.org (2005–2019)
6. Endometrial Hyperplasia; American College of Obstetricians and Gynecologists (2019)
7. Claudia T. Sadro; Imaging the Endometrium: A Pictorial Essay; Canadian Association of Radiologists Journal; 2016
8. Maryam Eftekhar, et al.; The thin endometrium in assisted reproductive technology: An ongoing challenge
9. E. Moschos, D. M. Twickler; Endometrial thickness predicts intrauterine pregnancy in patients with pregnancy of unknown location; International Society of Ultrasound in Obstetrics and Gynecology (ISUOG) (2008)
10. Jing Zhao et al.; The effect of endometrial thickness and pattern measured by ultrasonography on pregnancy outcomes during IVF-ET cycles; Reproductive biology and endocrinology: RB&E (2012)
11. Kevin S. Richter et al.; Relationship between endometrial thickness and embryo implantation, based on 1,294 cycles of in vitro fertilization with transfer of two blastocyst-stage embryos; Fertility and Sterility (2007)
12. Endometrial Hyperplasia; ACOG
Community Experiences
Join the conversation and become a part of our nurturing community! Share your stories, experiences, and insights to connect with fellow parents.
Read full bio of Dr. Sangeeta Agrawal
- Dr. Nandita Palshetkar is a gynecologist and IVF specialist with over 30+ years of experience. She is the scientific director at Blooms IVF clinic in Mumbai, India.
 Dr. Nandita Palshetkar is a gynecologist and IVF specialist with over 30+ years of experience. She is the scientific director at Blooms IVF clinic in Mumbai, India.
Dr. Nandita Palshetkar is a gynecologist and IVF specialist with over 30+ years of experience. She is the scientific director at Blooms IVF clinic in Mumbai, India.
Read full bio of shreeja pillai
Read full bio of Rebecca Malachi
Read full bio of Reshmi Das
















