Image: Shutterstock
The loss of a fetus before the 20th week of pregnancy is referred to as miscarriage, also known as spontaneous abortion or early pregnancy loss. Miscarriage rates might vary amongst women due to various factors.

This post discusses miscarriage statistics depending on age, weeks of pregnancy, chances of miscarriage during assisted reproduction, and statistics of recurrent miscarriages.
Key Pointers
- Most miscarriages occur in the first trimester.
- Consult a gynecologist to understand the reason and get timely treatment.
- It takes time to recover from a miscarriage, so seek doctor consultation.
How Many Pregnancies End In Miscarriage?
According to the US National Library of Medicine, spontaneous abortion or pregnancy loss may occur for approximately half of the pregnancies before the woman knows she was pregnant. About 10 to 15% of known pregnancies end in miscarriage (1).
Around 15% of miscarriages or fetal loss may happen in the second trimester, that is, between 13 and 19 weeks of pregnancy (2). Second-trimester miscarriages or fetal demise are often called late miscarriages. A pregnancy loss that happens after 20 weeks of gestation is called a stillbirth and is not included in statistics on miscarriage rates by weeks.
It is possible to have healthy pregnancies after a miscarriage too, and this is a natural process. You should try to understand it and not be emotionally affected by it. Medical termination of pregnancy (MTP) or medical abortions and self-induced abortions or self-induced miscarriages are not included in the rates mentioned above.
 Did you know?
Did you know?When Does Miscarriage Happen?
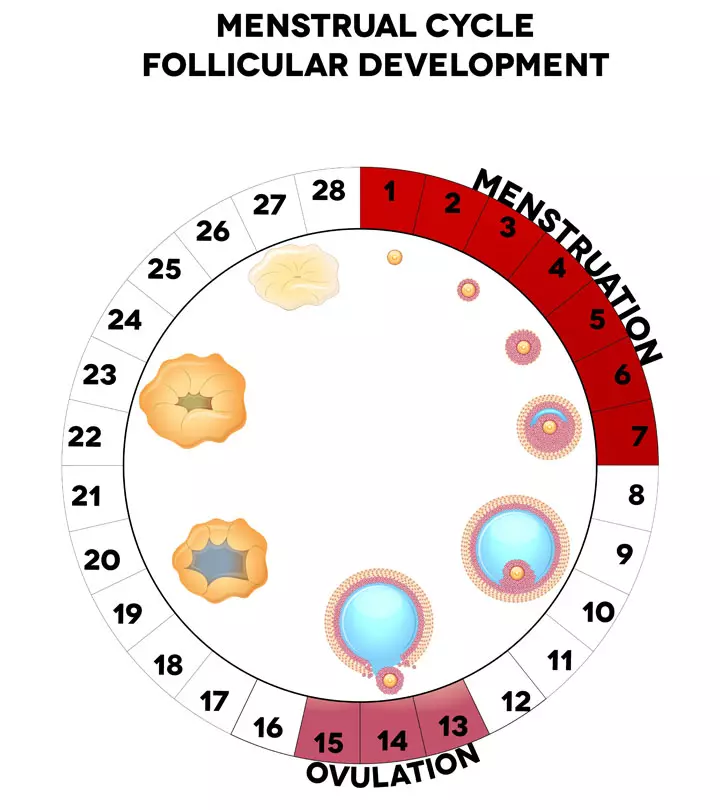
Most miscarriages tend to occur in the first trimester, that is, within the first 13 weeks, and this period accounts for around 80-85 % of all cases (3) (4). Among these, most incidences of miscarriages happen during the first seven weeks of pregnancy.
The risk of miscarriage can be higher or lower in each stage of pregnancy, depending on multiple maternal and fetal factors. Early pregnancy losses can be due to genetic factors, such as chromosomal abnormalitiesiA genetic condition caused by physical or numerical changes to one or more chromosomes that affect autosomes and sex chromosomes in the fetus. Early pregnancy loss factors are mostly beyond the control of women.
 Quick fact
Quick factWhat Are The Miscarriage Rates By Week?
The miscarriage rate may vary depending on multiple factors among women.
The relative risk of miscarriage by weeks of pregnancy can be the following (5) (6).
- 3-4 weeks: This is the time when implantationiAn early stage in fertilization when cells attach to the uterine wall occurs after the last menstruation, and pregnancy tests become positive. 50–75% of pregnancy loss happens before a positive pregnancy test, that is, before the fourth week. This is called chemical pregnancy and often indicated by other pregnancy and miscarriage symptoms.
According to gynecologist & obstetrician Dr. Nisarg Patel, “Chemical pregnancies are estimated to account for up to 75 percent of all miscarriages. Many women with a chemical pregnancy may not realize they are pregnant because they may have a normal or slightly delayed menstrual period. However, some may experience bleeding, cramping, or nausea.”
- 5th week: According to a study published in the American Journal of Epidemiology, the miscarriage rate can be around 21.3% (6). However, there can be a higher or lower risk of pregnancy loss depending on the maternal and fetal causes.
- 6–7 weeks: The rate of miscarriage during this week is about 5% since it is a point when the fetal heartbeat is obtained.
- 8–13 weeks: The miscarriage rate drops in this period to around 2–4%.
- 14–20 weeks: There is only a 1% chance of late pregnancy loss or late miscarriage during these weeks.
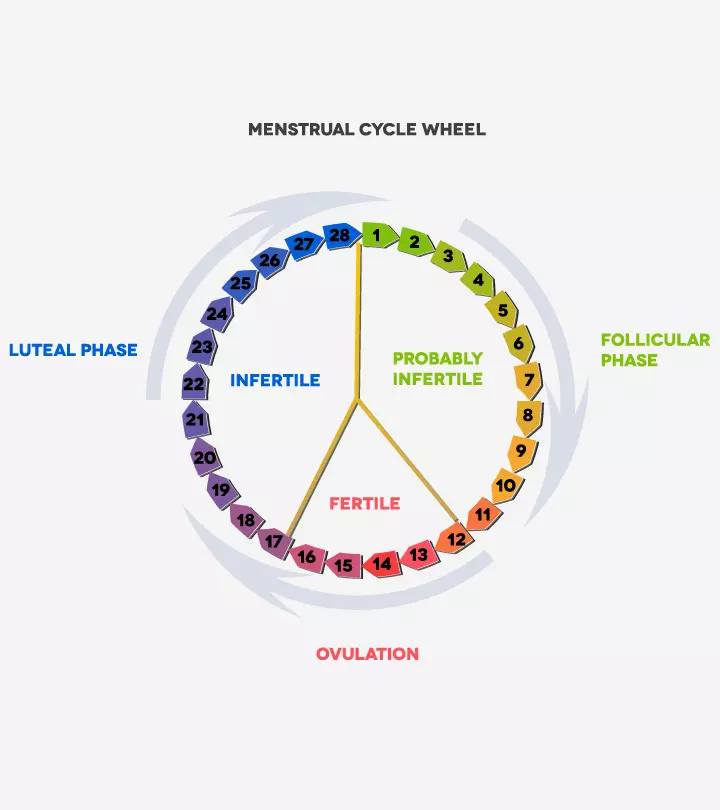
What Are The Miscarriage Rates By Age?
The miscarriage rate usually increases with age. The declining quality of ovum (egg) with increasing age could be one of the major causes of a higher incidence of pregnancy loss with advanced maternal age. The ovum has genetic problems in the form of chromosomal abnormalities.
The frequency of pregnancy loss for women at different ages is the following (3).
| Age | Frequency |
|---|---|
| 20–30 years | 9–17% |
| 35 years | 20% |
| 40 years | 40% |
| 45 years | 80% |
Note:
Paternal age over 35 years could also increase the risk of spontaneous abortion (7).
Research demonstrates that the pregnancy loss risk among women increases with maternal age, irrespective of reproductive history. Typically, it is lowest in women aged 19 years and below and highest in those aged 45 and above (16).
Understanding how age affects miscarriage rates can help expectant parents make better choices about family planning and timing. However, it is important to note that while the risk of miscarriage increases with age, many women still have healthy pregnancies.

Rates of miscarriage as women grow older
Source: Kaiser Family FoundationThe above-mentioned risk of miscarriage is purely based on maternal age. Several other risk factors, such as chronic illnesses, lifestyle, pregnancy complications, and hormonal changes, could also influence the miscarriage rate.
Risk Of Miscarriage And IVF
There is a chance of early pregnancy loss in 10-25% of the IVF-ET cycle (in vitro fertilizationiA process in which eggs from a woman's ovary are combined externally with sperms to create embryos and embryo transfer) (8). The pregnancy loss after an IVF procedure may affect you emotionally, physically, and financially since the pregnancy is not continued and often another IVF cycle is required.
Miscarriage is an indication that the embryo was implanted into the uterus. Biochemical pregnancy (positive pregnancy test) is also considered as a positive indicator for pregnancy.
Chromosomal anomalies could be a significant cause of spontaneous clinical abortions.
 Research finds
Research findsRecurrent Miscarriage Rate
Recurrent miscarriage, habitual abortion, or repeated pregnancy loss (RPL) is a loss of three consecutive pregnancies before 20 weeks from the last menstruation. A study published in the Reviews in Obstetrics and Gynecology shares that about 1–2% of women may experience repeated miscarriages, and it can leave many couples physically and mentally drained (9).
Repeated perinatal loss can be due to genetic factors, autoimmune conditionsiIt occurs when the immune system attacks the body instead of protecting it , infections, anatomical problemsiUnusual formations, sizes, or locations in the human body , or other unknown reasons. You may seek expert help to identify the cause and treatment to have a healthy pregnancy in the future.
 Quick fact
Quick factRisk Of Miscarriage After Fetal Heartbeat
The miscarriage rate declines at the point after the fetal heartbeat is detected on the ultrasound (1). Some studies suggest a 10% drop in the miscarriage rate by week once the baby’s heartbeat is detectable (10).
Many women may not be aware of fetal heartbeat until the first prenatal ultrasound scan by the 11th or 12th week. However, those who had fertility treatment may undergo scans earlier to accurately detect the risk of miscarriage based on the fetal heartbeat.
When Does The Risk Of Miscarriage Drop?
The pregnancy loss or miscarriage rate by week reduces when the pregnancy progresses. The risk of miscarriage may start to decline as early as when fetal heartbeats are detectable, which is around the 7th week pregnancy. However, a significant decline in the rate of miscarriage occurs after 12 weeks of gestation.
The drop in the miscarriage rate can also depend on other risk factors. For instance, chromosomal abnormalities could cause early pregnancy loss, while maternal factors like fibroidsiNon-cancerous growths that develop in or around the womb could result in late miscarriages.
 Did you know?
Did you know?What Should You Do If You Experience A Pregnancy Loss?
You may consult a gynecologist or any other doctor if you experience a miscarriage. They can give you the required treatment or help you identify the reason for pregnancy loss and resolve it.
The pregnancy tissue may not be expelled entirely during miscarriages in some cases. You may require an ultrasound examination to confirm the complete miscarriage. If any tissues are left in the uterus, then your doctor may initiate treatment to remove these tissues and avoid complications (3).
Miscarriage rates by week may vary depending upon several maternal and fetal factors. Nonetheless, if you have excessive bleeding and signs of infection during pregnancy, you must seek immediate medical attention. Your doctor may advise preventive measures, such as administering Rh immunoglobuliniProteins in the body that fight germs, also known as antibodies , if you have an Rh-negative blood type to reduce the risk of complications in your subsequent pregnancies.
Frequently Asked Questions
1. How can I stop worrying about miscarriage?
Many women may have anxiety about experiencing a miscarriage or threatened miscarriage when pregnant, especially those who have experienced it. According to the American Pregnancy Association (APA), 85% of women who had one loss and 75% of women who had two to three losses go on to have a successful pregnancy next time. If the fear and anxiety are causing a lot of mental distress, you may discuss your apprehensions with your OB/GYN or mental health specialist (11).
2. What does not cause miscarriage?
Many women have misconceptions that excess workouts, vomiting, stress, physical strain, and birth control pills cause miscarriage. Though excess consumption of alcohol and drugs could be responsible for miscarriage, other factors mentioned above do not cause it (3).
3. Am I more fertile after a miscarriage?
A study by the US National Institutes of Health (NIH) found that women who try to conceive three months after a loss may conceive sooner than those who try after three months. You can try for a pregnancy after miscarriage as soon as your doctor clears you and you are emotionally ready (12).
4. How painful is a miscarriage?
A miscarriage may cause cramps and abdominal pain, which is usually more severe than menstrual cramps. It may be accompanied by mild to severe low back pain (13).
5. How do one confirm a miscarriage at home?
Bleeding that becomes progressively heavy along with severe abdominal cramps, may indicate a miscarriage. Grayish tissue or blood clots may be passed. A decrease in pregnancy symptoms may further add to the indication. However, you should immediately contact your healthcare provider and get yourself examined (13).
6. What lifestyle changes can help reduce the risk of miscarriage?
To help reduce the chances of miscarriage, you can make some simple changes in your life. Stop smoking and drinking alcohol, eat healthy foods like fruits and vegetables, and try to reach a healthy weight before getting pregnant. Obstetrician and gynecologist Dr. Veena Madhankumar suggests, “To reduce the risk of miscarriage, manage stress and anxiety, limit caffeine intake, take prenatal vitamins, attend regular prenatal checkups, and avoid exposure to pesticides, radiation, and certain harmful chemicals that can affect pregnancy.” You may also exercise gently and find ways to relax, such as doing yoga. Get enough sleep and stay away from harmful chemicals. While these steps can help, remember that not all miscarriages can be prevented.
However, the duration of recovery from a miscarriage differs from one woman to another. Also, it may take time for you to regularize your period cycles, depending on your pregnancy stage and other factors. It is essential to consult your healthcare provider before you plan your next pregnancy and consider consuming essential prenatal vitamins and supplements in advance to retain a healthy pregnancy.
Infographic: Talking To Someone Who Experienced A Miscarriage
A miscarriage is a disheartening event. A strong support system is pivotal in helping the grieving woman cope with loss. Here is an infographic that can help you learn what you should and should not tell a woman who experienced a miscarriage.
Some thing wrong with infographic shortcode. please verify shortcode syntax
Illustration: Miscarriage Rates By Week And Risks Involved

Image: Dall·E/MomJunction Design Team
Pregnancy is a beautiful thing and you may wonder what precautions are necessary during this time and when you must be extra careful. Watch this informative video to learn when and how miscarriages usually occur.
References
1. Miscarriage; MedlinePlus; The United States National Library of Medicine
2. Thomas C. Michels; Second Trimester Pregnancy Loss; The American Academy of Family Physicians
3. Early Pregnancy Loss; The American College of Obstetricians and Gynecologists
4. Miscarriage: your questions answered; NCT (National Childbirth Trust)
5. Miscarriage ; Centers For Disease Control And Prevention
6. Sudeshna Mukherjee, et al.; Risk of Miscarriage Among Black Women and White Women in a US Prospective Cohort Study; The American Journal of Epidemiology (2013).
7. Riffat Jaleel and Ayesha Khan; Paternal factors in spontaneous first trimester miscarriage; Pakistan Journal of Medical Sciences (2013).
8. G.Wright Bates Jr and Elizabeth S Ginsburg; Early pregnancy loss in in vitro fertilization (IVF) is a positive predictor of subsequent IVF success; The American Society for Reproductive Medicine and Canadian Fertility and Andrology; Fertstert
9. Holly B Ford and Danny J Schust; Recurrent Pregnancy Loss: Etiology, Diagnosis, and Therapy; Rev Obstet Gynecol (2009).
10. Stephen Tong, et al.; Miscarriage Risk for Asymptomatic Women After a Normal First-Trimester Prenatal Visit; Obstet Gynecol (2008).
11. Pregnancy After Miscarriage; American Pregnancy Association.
12. Trying to conceive soon after a pregnancy loss may increase chances of live birth; National Institutes of Health
13. Miscarriage; Cleveland Clinic
14. Maya Sharon-Weiner et al.; Conception after early IVF pregnancy loss: should we wait?; NCBI (2025)
15. Miscarriage; National Library Of Medicine
16. Gabriela Weigel et al.; Understanding Pregnancy Loss in the Context of Abortion Restrictions and Fetal Harm Laws; Kaiser Family Foundation
Community Experiences
Join the conversation and become a part of our nurturing community! Share your stories, experiences, and insights to connect with fellow parents.
Read full bio of Dr. Surveen Ghumman Sindhu
- Dr. Nisarg Patel is a gynecologist, obstetrician, and laparoscopic surgeon from Ahmedabad, India, with over 13 years of experience in the field. He did his post graduation in Obstetrics and Gynecology from Pravara Institute of Medical Sciences, Ahmednagar, and holds a fellowship of Reproductive Medicine.
 Dr. Nisarg Patel is a gynecologist, obstetrician, and laparoscopic surgeon from Ahmedabad, India, with over 13 years of experience in the field. He did his post graduation in Obstetrics and Gynecology from Pravara Institute of Medical Sciences, Ahmednagar, and holds a fellowship of Reproductive Medicine.
Dr. Nisarg Patel is a gynecologist, obstetrician, and laparoscopic surgeon from Ahmedabad, India, with over 13 years of experience in the field. He did his post graduation in Obstetrics and Gynecology from Pravara Institute of Medical Sciences, Ahmednagar, and holds a fellowship of Reproductive Medicine. 
Dr. Veena Madhankumar is an experienced obstetrician and gynecologist with 25 years of clinical expertise. She completed her MBBS from Coimbatore Medical College, India, in 1999 and pursued her MD in Obstetrics and Gynecology from Sri Ramachandra Medical College, Chennai, India. Dr. Madhankumar has been associated with iCliniq for over a decade, providing expert medical consultations and guidance. She has also established a practical laparoscopy training course.
Dr. Veena Madhankumar is an experienced obstetrician and gynecologist with 25 years of clinical expertise. She completed her MBBS from Coimbatore Medical College, India, in 1999 and pursued her MD in Obstetrics and Gynecology from Sri Ramachandra Medical College, Chennai, India. Dr. Madhankumar has been associated with iCliniq for over a decade, providing expert medical consultations and guidance. She has also established a practical laparoscopy training course.
Read full bio of Dr Bisny T. Joseph
Read full bio of Rebecca Malachi
Read full bio of Aneesha Amonz