Image: MomJunction Design Team

Key Pointers
- The fetal position can affect the ease or difficulty of the childbirth process.
- A head-first position is ideal for a vaginal birth, but other positions may require alternate delivery methods.
- Occiput anterior, occiput posterior, occiput transverse, breech, and umbilical cord presentation are the types of fetal positions.
- Breech positions increase the risk of umbilical cord complications and may require an assisted delivery.
- Fetal positions can determine the delivery method and serve as an indicator of the health of both the mother and baby.
Why Is The Fetal Position Important?
The fetal position can determine the ease or difficulty of your childbirth. Your infant may assume one of various possible baby birth positions by the end of the gestation period, which is also a deciding factor for a vaginal birth or cesarean delivery.
If your baby has transitioned to a head-first position by the end of the term, they can descend through your vaginal opening without difficulty during delivery.
This post discusses the various fetal positions your baby may present in when you’re in labor and its impact on the delivery process.
Different Fetal Positions During Pregnancy
Before the due date, your baby will drop down into the pelvis. Here are the different positions your baby can get into when you are preparing for your delivery.
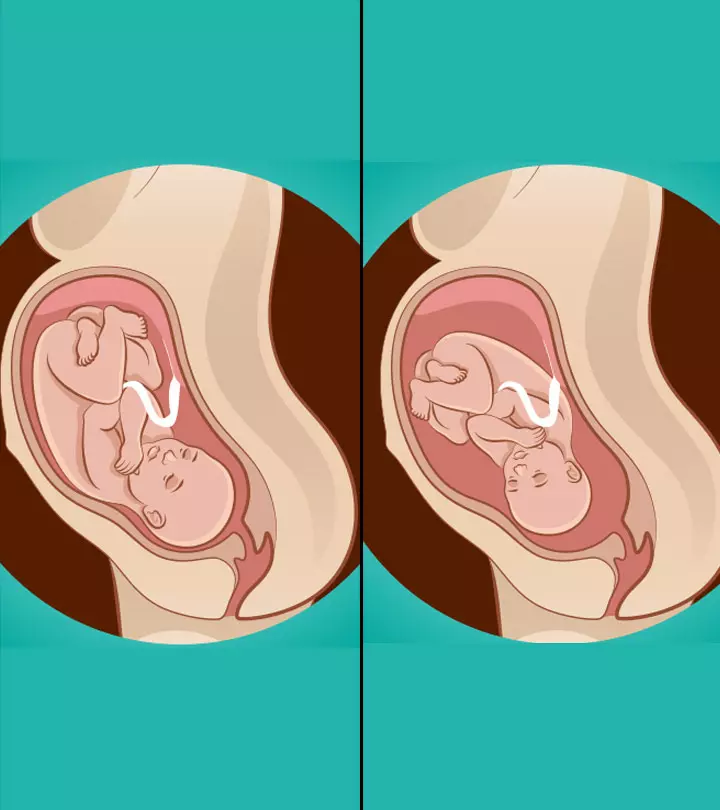
1. Occiput anterior (OA)

This is the ideal position your baby could attain towards delivery. The baby moves into the pelvis with her head-down, facing the mother’s back with chin tucked to the chest. Her head points towards the birthing canal. This is called the longitudinal lie.
Termed the vertex presentation of the fetus, this position is generally attained between 32nd and 36th weeks of gestation (1). The baby will stay in the same position for the rest of your pregnancy. This position is considered ideal for the baby to come out of the birthing canal with head first.
There are two more presentations in the OA position:
i. Face and brow presentation: The baby will remain in the OA position, but her face and not head will be pointing towards the birth canal. This happens when her chin is pointing outward instead of being tucked against the chest. The obstetrician can identify this position during a vaginal examination, by feeling the bony jaws and the mouth of the baby (2).
In brow presentation, the baby will be in the OA position but her forehead will be pointing towards the birth canal. During the vaginal examination, the doctor can feel the anterior fontanelleiA soft space between the bones of an infant's skull (yet to develop) typically seen after birth and the orbits of the forehead (2)
Neonates, who are in the face and brow position during vaginal birth, are often presented with facial edema (facial swelling), bruising, or soft tissue trauma (8).
ii. Compound presentation: The baby is positioned anteriorly with one of her arms lying along her head pointing towards the birthing canal. The arms may slide back during the delivering process, but when they don’t, then extra care needs to be taken while taking out the baby safely. Additionally, there is an increased risk of umbilical cord prolapse in such presentations (8).
A study published by the Society for Academic Specialists in General Obstetrics and Gynecology (SASGOC) states that face, brow, and compound fetal presentations complicate about 3-4% of all term births (8).
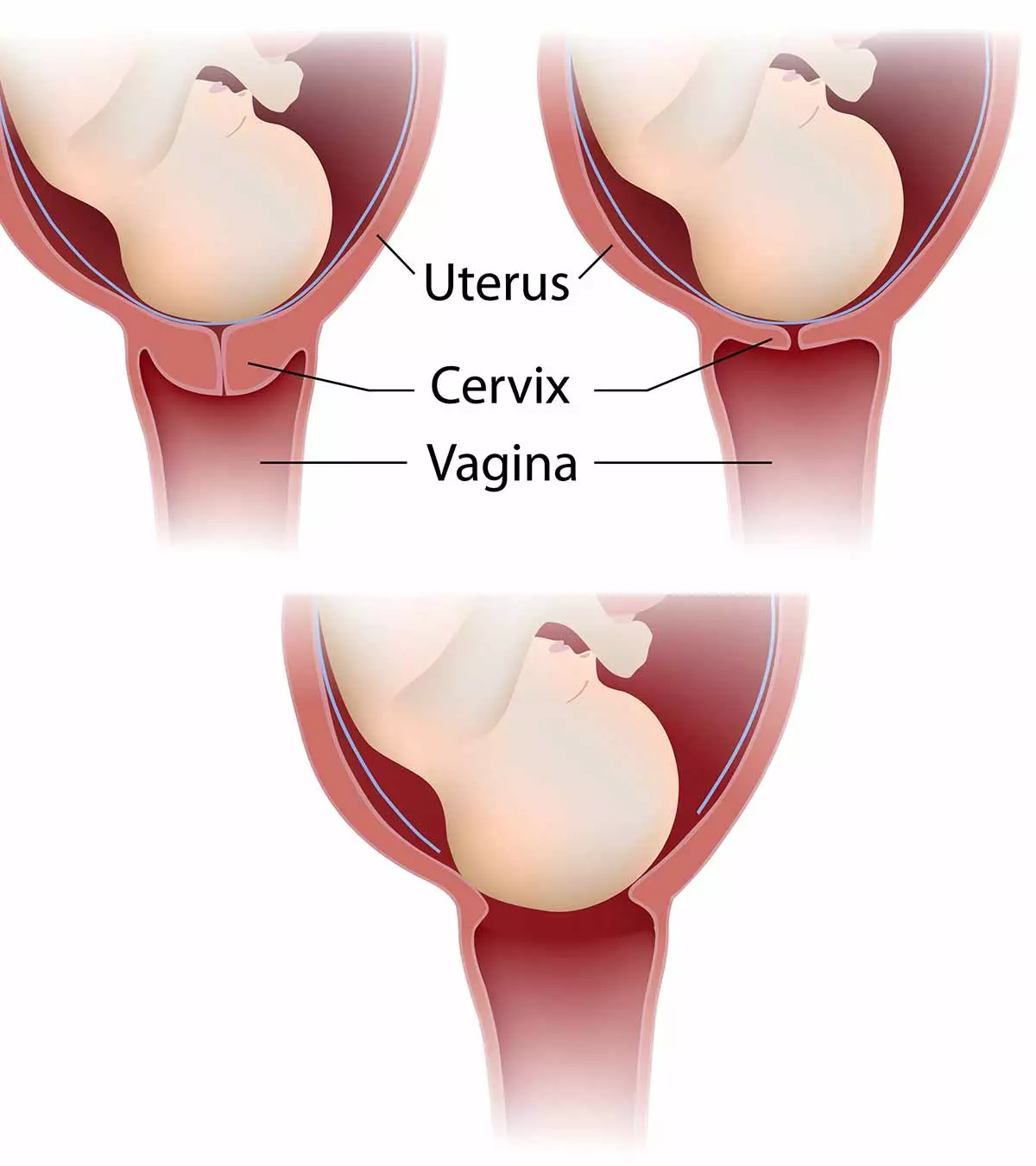
2. Occiput posterior (OP)

The baby moves into the pelvis with her head-down but facing the front/abdomen of the mother. This position is also known as ‘sunny-side up’ or ‘face up’ position. OA and OP are called the cephalic or head-first positions.
Generally, around 10-34% of babies remain in occiput posterior position during the first stage of labor and then turn to the optimal (OA) position. But, some remain in this position, which can make labor difficult, resulting in emergency C-section. Statistical reports released by the Centers for Disease Control and Prevention (CDC) suggest that about 32.1% of all deliveries in the US are cesarean (20).
This fetal position can prolong your labor, lead to instrumental interventions, severe perineal tearsiA minor vaginal stretch or injury that often happens during vaginal birth or a C-section (3).
3. Occiput transverse (OT)
The baby lies sideways in the womb (1). If she fails to turn to the optimal position at the time of delivery, then a C-section becomes necessary. During the vaginal examination, the doctor can sometimes feel the shoulder, or the arm, elbow or hand prolapsing into the vagina. This position also poses the risk of umbilical umbilical cordiA tube-like structure that delivers oxygen and nutrition to the fetus in the womb prolapse, in which the umbilical cord comes out before the baby. As per some studies, the incidence of a cord prolapse in a transverse lie position is around 9%, which is a medical emergency and needs an immediate C-section (21).
In some cases, assisted delivery is carried out by rotating the baby manually or using forceps or a vacuum to turn the baby into the ideal position (22).
4. Breech position

In this fetal presentation, the baby is positioned with her head up and buttocks pointing towards the birthing canal. This occurs in about 3-5% of all full-term deliveries. Also, the risk of breech presentation in subsequent deliveries increases by nearly 10% in the second pregnancy, 27% in the third pregnancy, and so on. There are three different variations of breech presentations (23) (24):
i. Complete breech: The buttocks point towards the birthing canal with the legs folded at the knees and the feet positioned near the buttocks. This position increases the risk of umbilical cord loop in a vaginal delivery. Moreover, the cord could pass through the cervix before the head, causing injuries to the baby.
Shelley Dobbin, a mother, talks about her experience with her baby being in the breech position. She says, “At my 37-week antenatal appointment, my Midwife noticed that our baby was in the breech position. My Midwife had to consult with the doctors who wanted to perform an External Cephalic Version (ECV) on me. An ECV is a procedure in which doctors use their hands on your tummy to try to manually turn the baby into a head-down (cephalic) position… I ended up booking the External Cephalic Version… The ECV failed. They moved Baby Dobbin into a head-down position, but our baby immediately turned its body all the way back into the breech position.”
She then shares her experience of how she decided against a cesarean section, which was suggested by the doctors, and managed to have a successful vaginal birth (i).
ii. Frank breech: The buttocks point towards the birth canal with the legs stretching straight up and feet reaching the head. This can also lead to umbilical cord loop, causing injuries to the baby while attempting a vaginal birth; however, it is uncommon with an incidence rate of 0.5%.
iii. Footling breech: The baby’s buttocks are downwards, with one of her feet pointing towards the birthing canal. This fetal presentation is at the highest risk of umbilical cord prolapse at 15-18%, which could even cut off the blood supply and oxygen to the fetus.
5. Umbilical cord presentation

During this, the umbilical cord comes out first through the birthing canal (4). However, there is a difference between umbilical cord presentation and prolapse based on the condition of the uterine membrane.
Whereas a cord presentation happens when the umbilical cord enters the birthing canal before the water breaks, a cord prolapse occurs after the water breaks, which calls for an immediate C-section (25).
The positions are influenced by the health condition of the mother and the baby.
What Are The Risk Factors For Having A Difficult Fetal Position?
The below factors increase the risk of fetal malpositions (5):
Maternal factors:
- In high parity women, who had more than five pregnancies of less than 20 weeks gestation (6), the abdominal wall muscle tone fails to hold the baby in a stable longitudinal lie.
- Placenta previa, where the placenta blocks the cervical opening.
- Placenta contracture occurs when the stretchy tissues are replaced by non-stretchy tissues.
- Pelvic tumors such as an ovarian cyst during pregnancy or uterine tumors.
- Uterine malformations like uterus cordiformis, subseptus, or septus and uterus unicornisiA rare hereditary condition where only half of the uterus is present in a woman, increasing the risk of pregnancy complications , bicornis, and didelphys can cause space restriction inside the uterus.
- Distended urinary bladder.
Fetal factors:
- Polyhydramnios – excess amniotic fluid in the birth sac — helps the fetus move freely in the womb, making it unstable and resulting in its malpositioning.
- Oligohydramnios – the deficiency of amniotic fluid — restricts the fetal movements.
- If the mother is carrying multiple fetuses, one or both the fetuses might change their position frequently, leading to malpositioning.
- Fetal abnormalities, such as hydrocephaly (tumors of the fetal neck or sacrum), fetal abdominal distention as with hydrops fetalis, and fetal neuromuscular dysfunctioniA group of conditions affecting the fetal muscles and nerves, leading to muscle weakness and neurological disorders , can prevent the fetus from engaging properly into the maternal pelvis.
These factors increase the likelihood of having an unsuitable fetal position but you don’t have to lose hope.
 Quick fact
Quick factCan The Fetal Position Be Corrected?
Yes. There are two ways to correct the position of your baby. They are described below:
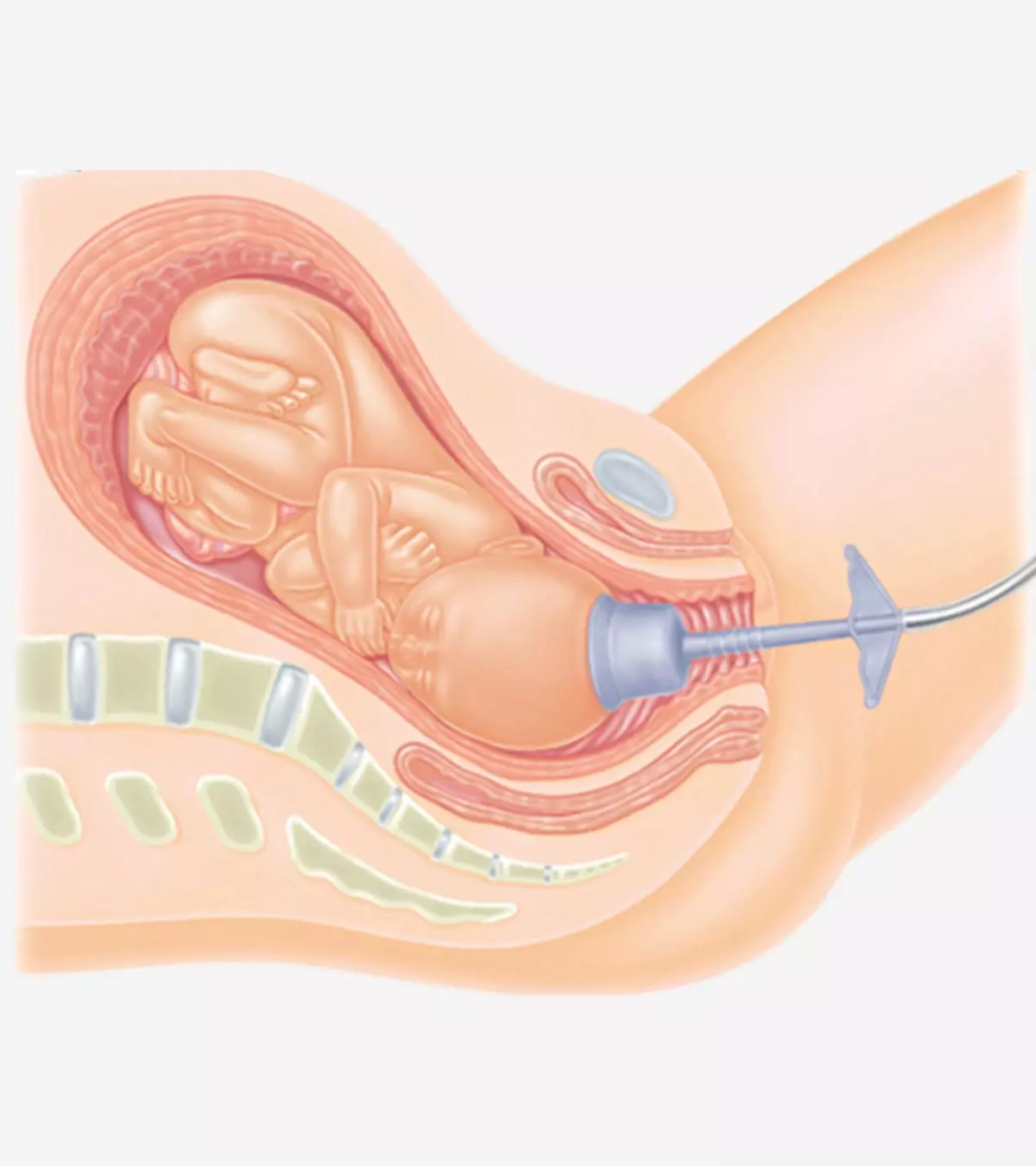
1. External cephalic version (ECV)
This medical procedure is undertaken after 37 weeks of pregnancy. The technique involves rotating the baby by applying pressure on the abdomen. The doctor places one hand over the head of the baby and the other hand on the buttocks to turn her to the optimal position.
During this procedure, the heartbeat of the baby will be closely monitored using an ultrasound. In the case of any discrepancy in the fetal heart rate, the procedure will be stopped immediately.
This procedure may or may not work. Studies show that about 1 in 1,000 women goes into labor after an ECV while about 1 in 200 women need an immediate C-section (7).
 Did you know?
Did you know?ECV is not recommended in the cases of:
- Multiple pregnancies
- Unusual shape of uterus
- Recent vaginal bleeding
- Low levels of amniotic fluid
- Placenta previa
- Complicated pregnancy
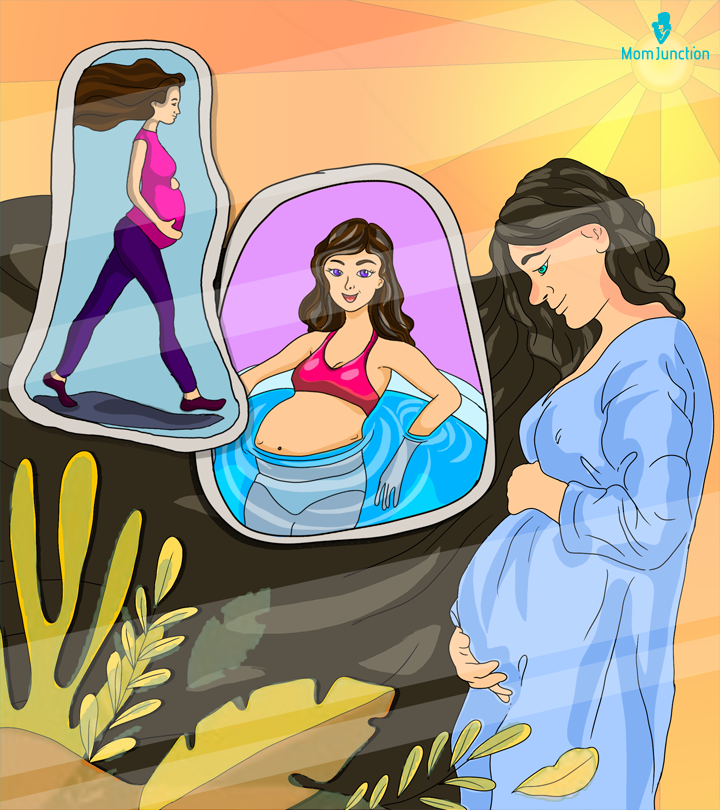
2. During labor
Most babies turn to an ideal birthing position with the onset of labor and eventually the baby’s head will start crowning. If it doesn’t happen, if the baby doesn’t engage during labor, or if the shape of the pelvis is not favorable for vaginal birthing, then a Cesarean-section is performed. Practicing breathing and relaxation exercises may help with pain management. Your doctor may also administer an epidural to relieve the pain. Additionally, activities like listening to music and talking to the fetus may stimulate the fetus in the womb to change position. Moreover, a chiropractic technique, known as the Webster technique, and acupuncture from a licensed professional can also help (1).
 Point to consider
Point to considerHow Is Belly Mapping Done?
Belly mapping is a method for you to track the position of your baby. You can do this from the eighth month of pregnancy. However, make sure to talk to your doctor before doing it.
Things you require: A marker (the ink stain should be easy to remove)
How to do:
- Lie down, draw a circle on your tummy and divide it into four parts.
- Feel the movements of the baby. Try to feel the baby’s head by slightly putting pressure on your abdomen. The point where you feel a ball like feature, mark it as the head on your belly.
- Use a fetoscope to hear your baby’s heartbeat and mark the point. You will feel a long hard mass, which indicates the back of your baby. The heart is the part of this long mass.
- Next, try to find the bum, which feels like a hard part. Mark this point on your belly.
- Now feel the kicks and wiggles as they give you a clue about the location of the baby’s legs and knees. Mark it too.
- Join all the points you have marked to find the position of your baby.
Belly mapping is complicated, and you may or may not be able to track the baby’s movements accurately. Therefore, take help and support from the father, doula, or your family. Alternatively, you may club it with a few other ways.
Other Ways To Know The Position Of The Baby
Here are a few indications:
| Indications | Likely fetal position |
|---|---|
| Feel the baby’s kicks under the ribs with your navel popping out | Anterior position with head-down |
| Feel the kicks at the front of the tummy and the tummy seems flattened | Posterior position |
| Push the lump on your bump and feel the whole baby moving | The lump is the bottom of the baby. Determine the position based on the location of that lump |
| Lump on one side that moves by itself without any change in the positioning of the rest of the body | The lump is the head of your baby. You can determine the position based on the position of the lump |
| Feel the hiccups at the bottom of the belly | Head-down position |
| Feel the hiccups above the belly button | Head-up position |
| Extreme pain under the ribs | Head-up position |
| Heartbeats felt above belly button | Head-up |
| Heartbeats felt below belly button | Head-down |
These are mere speculations, but also a means to enhance bonding with the infant. They do not replace your doctor’s advice. The doctors may suggest an intrapartum ultrasound to learn about your fetus’ position and presentation, in addition to fetal attitude. This will help them to make decisions about your mode of delivery (26).
Frequently Asked Questions
1. Can a baby’s position during birth impact their health in the long term?
A baby’s position in the womb, especially in cases of breech, could lead to injuries such as dislocated or broken bones. In addition, breech babies’ birth defects might include umbilical cord flattening or twisting, which may lead to brain damage from the lack of blood or oxygen supply during birth, affecting the long-term health of the newborn (10).
2. Can maternal posture affect the birth position of the baby?
Studies indicate that maternal posture during pregnancy does not affect the baby’s fetal position before birth. However, studies suggest that the birthing position assumed by the mother influences the childbirth process and the positioning of the baby, as some positions may not provide adequate room for the baby to turn itself while others may. Sitting, squatting, hands and knees posture and lying on the side may help in getting the baby in the best position during labor. (11) (12).
3. Are there any benefits to using certain birth positions?
Specific birthing positions might make the birthing process easier for both the mother and the baby. For example, the upright position reduces the risk of compressing the aorta, provides more oxygen supply, contracts the uterus strongly, and helps the baby get in a better position (13).
4. Which position is most commonly used for giving birth?
The most common birthing position in the US is the reclining position, where the mother is laid on her back with the head of the bed lifted for her comfort (14).
5. Can birth positions affect the speed of labor?
Some studies have shown that the standing, lateral, forward bending, flexible sacrum birthing and exaggerated lithotomy positions might help fasten fetal head descent. However, the comfort of the mother should also be taken into account, and she should choose the position that suits her the best (11) (12) (13) (15)
6. Is it possible to change positions during labor?
A few studies have found movement and change in position during labor to be helpful. Bringing about a change in positions helps women cope with the pain of labor and moves the pelvic bones, allowing the baby to find the best position and fit (16).
7. How do partners or support people assist mothers in different birth positions during delivery?
Partners or support people help women during their delivery by encouraging and reassuring them, praising them for their efforts, helping them breathe, rubbing their back for relaxation, providing water as and when allowed, and wiping their forehead and brows for some relief (17).
8. How can you promote optimal fetal positioning?
The best way for your baby to come out is head first, facing your back. Try getting on your hands and knees, lying on your side, or sitting on a low seat or exercise ball (18). A study found that when mothers lay on their side (semi-prone) or got on their hands and knees (knee-chest position), it helped babies to turn into the right position for birth. These positions also made it more likely for mothers to have a natural birth and feel less back pain during labor (19).
A woman has multiple choices for giving birth, such as natural delivery, water birth, or cesarean section. However, the position of the baby during the gestation period ultimately determines whether a vaginal or C-section delivery is required. Hence, it is good to understand the various possible baby birth positions to prepare for different birthing scenarios. Positions such as occiput posterior, occiput transverse, and the breech position may necessitate a cesarean delivery. Fortunately, the fetus returns to the ideal birthing position before labor in many cases. If this does not happen, your doctor or midwife will advise you on the best manner to proceed that’s safe for the mother and child.
Infographic: When Does Cesarean Section Is Indicated For Fetal Malpresentation And Malposition?
Fetal malpresentation is when the baby does not present head-first in the birth canal. Fetal malposition consists of abnormal head positions during labor. Cesarean section is often suggested if there is a possibility of fetal malposition or malpresentation that could delay labor to avoid permanent injuries. Go through the infographic to know the indications for emergency cesarean sections in fetal malpresentation and malpositions. Illustration: Momjunction Design Team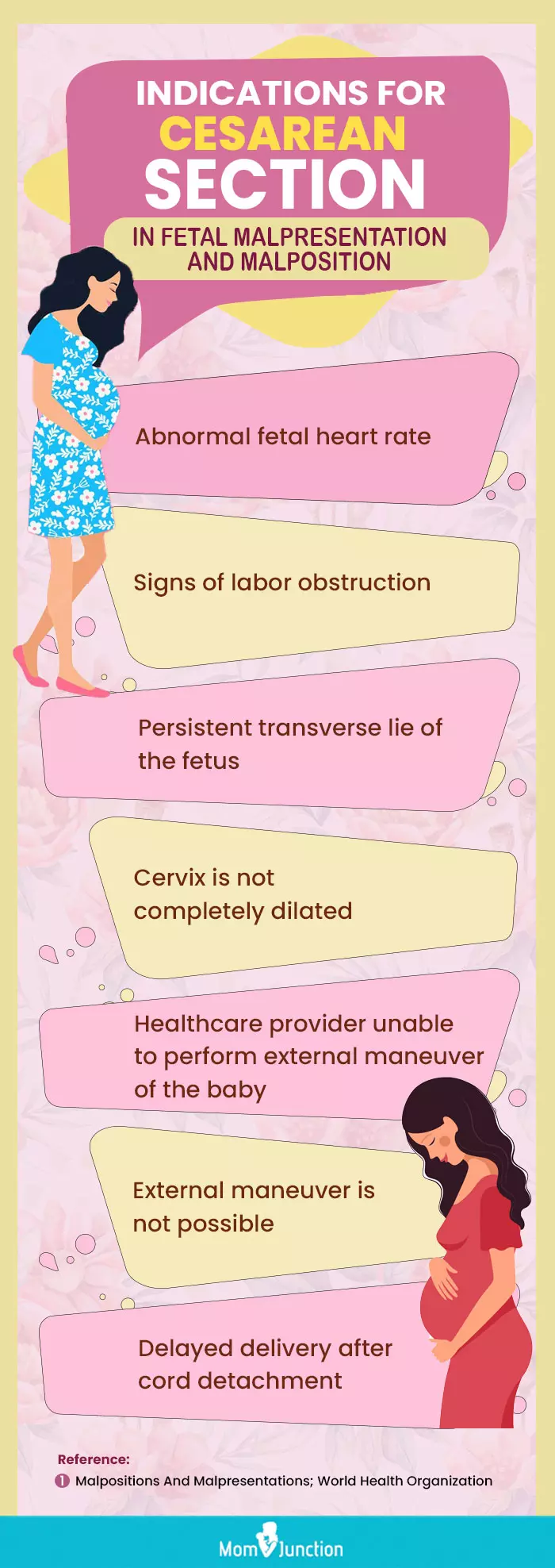
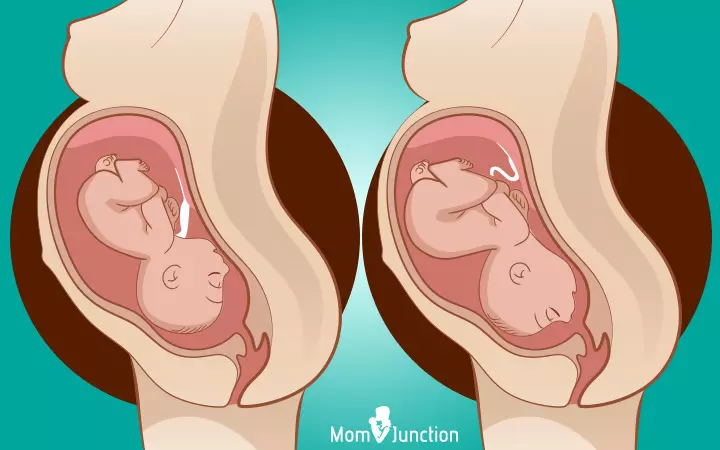
Illustration: What Are The Best Baby Birth Positions For Comfortable Delivery?

Image: Dall·E/MomJunction Design Team
Learn effective techniques to facilitate a more comfortable childbirth. Acquire expert advice on optimal positions to assist during labor. Expand your understanding for a successful delivery.
Personal Experience: Source
MomJunction articles include first-hand experiences to provide you with better insights through real-life narratives. Here are the sources of personal accounts referenced in this article.
i. An informed and educated breech birth.https://birthwithoutfearblog.com/2011/07/12/an-informed-and-educated-breech-birth/
References
- Fetal Positions for Birth.
https://my.clevelandclinic.org/health/articles/9677-fetal-positions-for-birth - Julija Makajeva and Mohsina Ashraf (2025). Delivery Face And Brow Presentation.
https://www.ncbi.nlm.nih.gov/books/NBK567727/ - Marie-Julia Guittier et al. (2014) Maternal positioning to correct occipito-posterior fetal position in labour: a randomised controlled trial
https://bmcpregnancychildbirth.biomedcentral.com/articles/10.1186/1471-2393-14-83
- Cord Presentation and Prolapse.
https://www.gfmer.ch/Obstetrics_simplified/cord_presentation_and_prolapse_.htm - Unstable lie of the fetus.
https://www.sahealth.sa.gov.au/wps/wcm/connect/249e33804eee75fdbef8bf6a7ac0d6e4/Unstable+lie+of+the+fetus_PPG_v4_1.pdf?MOD=AJPERES&CACHEID=ROOTWORKSPACE-249e33804eee75fdbef8bf6a7ac0d6e4-nGF9Ok - Yahya M Al-Farsi, et al., (2012), Effect of high parity on occurrence of some fetal growth indices: a cohort study.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3410699/ - External cephalic version (ECV)
https://www.pregnancybirthbaby.org.au/external-cephalic-version-ecv - Management of Brow, Face, and Compound Malpresentations.
https://exxcellence.org/list-of-pearls/management-of-brow-face-and-compound-malpresentationshttps://exxcellence.org/list-of-pearls/management-of-brow-face-and-compound-malpresentations - If Your Baby Is Breech.
https://www.acog.org/womens-health/faqs/if-your-baby-is-breech - Breech Baby
https://my.clevelandclinic.org/health/diseases/21848-breech-baby - Hunter and Kulier; (2007); Hands and knees posture in late pregnancy or labour for fetal malposition (lateral or posterior).
https://pubmed.ncbi.nlm.nih.gov/17943750/ - Huang et al; (2019); A review and comparison of common maternal positions during the second-stage of labor
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6839002/ - Marta Berta et al; (2019); Effect of maternal birth positions on duration of second stage of labor: systematic review and meta-analysis
https://bmcpregnancychildbirth.biomedcentral.com/articles/10.1186/s12884-019-2620-0 - 5 Different Birthing Positions to Try During Labor
https://www.lancastergeneralhealth.org/health-hub-home/motherhood/your-pregnancy/5-different-birthing-positions-to-try-during-labor# - Mahboubeh Valiani; et al.; (2016); Comparative study on the influence of three delivery positions on pain intensity during the second stage of labor
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4979260/ - Michele Ondeck; (2014); Healthy Birth Practice #2: Walk Move Around and Change Positions Throughout Labor
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4235058// - Support during Labour and Childbirth
https://www.ncbi.nlm.nih.gov/books/NBK304186/ - Journey of Labour
https://www.qld.gov.au/health/children/pregnancy/antenatal-information/journey-of-labour/getting-baby-in-the-right-position-for-birth - Hadis Bahmaei et.al; (2025); The Impact of Maternal Position in Labor on Occiput-Posterior Position of Fetus and Pregnancy Outcomes in Pregnant Women Without Epidural Analgesia
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10397531/ - Births: Final Data for 2025.
https://www.cdc.gov/nchs/data/nvsr/nvsr72/nvsr72-01.pdf - Marybeth Lore; (2017); Umbilical Cord Prolapse and Other Cord Emergencies.
https://www.glowm.com/section-view/heading/Umbilical%20Cord%20Prolapse%20and%20Other%20Cord%20Emergencies/item/136 - Bradley de Vries et al.; (2015); Transverse occiput position: Using manual Rotation to aid Normal birth and improve delivery OUTcomes (TURN-OUT): A study protocol for a randomised controlled trial.
https://pmc.ncbi.nlm.nih.gov/articles/PMC4539677/ - Caron J. Gray and Meaghan M. Shanahan; (2025); Breech Presentation.
https://www.ncbi.nlm.nih.gov/books/NBK448063/ - Breech Births.
https://americanpregnancy.org/healthy-pregnancy/labor-and-birth/breech-presentation/ - Umbilical Cord Prolapse (Green-top Guideline No. 50).
https://www.rcog.org.uk/guidance/browse-all-guidance/green-top-guidelines/umbilical-cord-prolapse-green-top-guideline-no-50/ - Alexis C. Gimovsky; Intrapartum ultrasound for the diagnosis of cephalic malpositions and malpresentations.
https://www.ajogmfm.org/article/S2589-9333(21)00133-6/abstract
Community Experiences
Join the conversation and become a part of our nurturing community! Share your stories, experiences, and insights to connect with fellow parents.
Read full bio of Dr. Sangeeta Agrawal
Read full bio of Sakshi Mishra
Read full bio of Rebecca Malachi
Read full bio of Aneesha Amonz