Image: Shutterstock
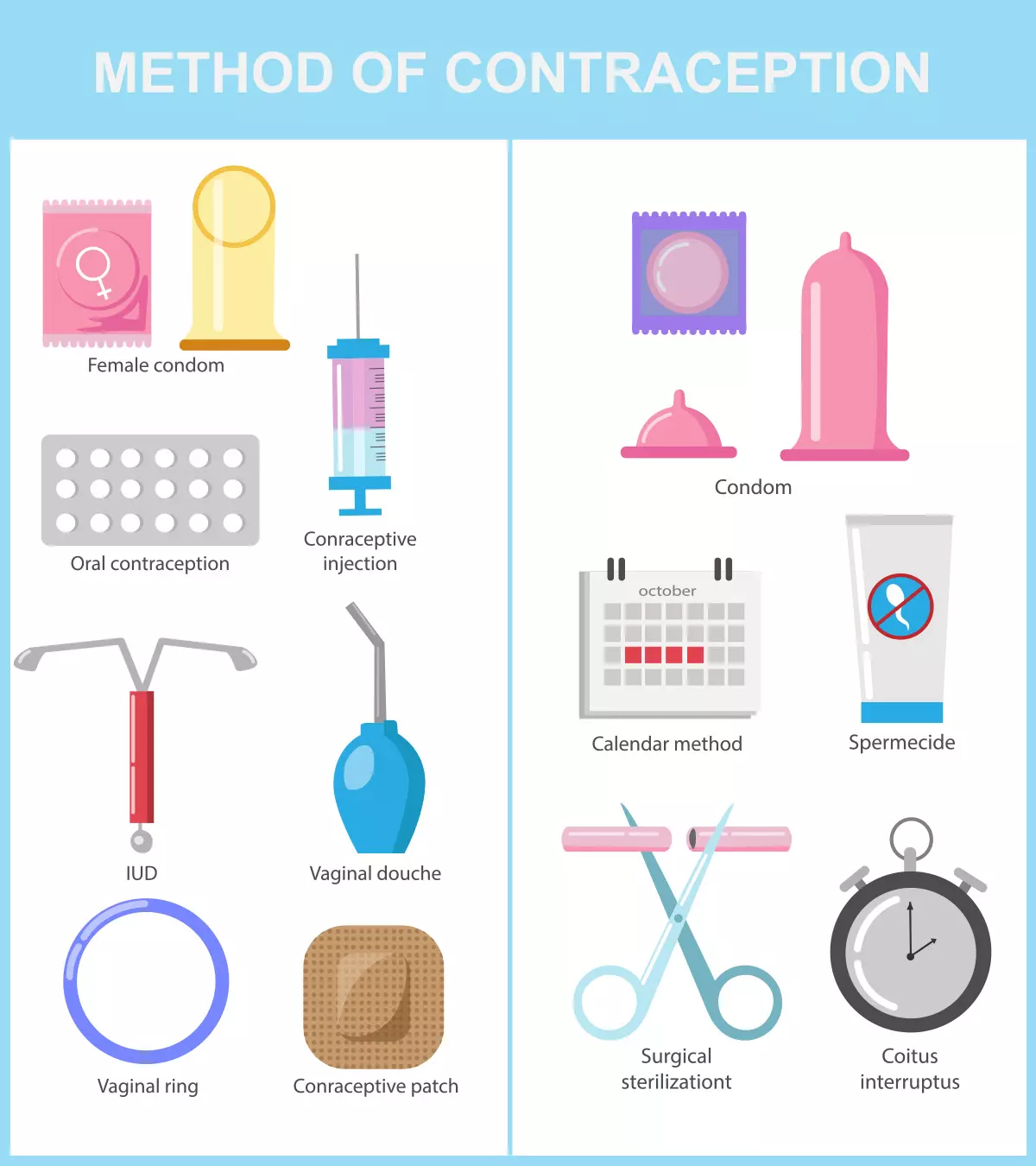
Unplanned pregnancies can cause difficulties both for the parents and the baby. Thus, in this post, we discuss some effective pregnancy prevention methods to help you avoid an unintended pregnancy.

Every time you have made love without protection, you carry a possibility of getting pregnant. Therefore, if you do not intend to start a family or get pregnant any time soon, you should use contraceptives such as hormonal or non-hormonal medicines, birth control devices, or natural techniques (1).
Read on as we tell you more on how to prevent pregnancy using different contraceptive methods, their benefits, and side effects.
Key Pointers
- Effective methods of avoiding pregnancy include hormonal contraceptives such as implants, injections, birth control patches, vaginal rings, and progestin-only pills.
- Hormonal contraceptives work by inhibiting ovulation, delivering synthetic hormones into the blood, or altering the texture of cervical mucus.
- Sterilization through surgical methods is a safe and permanent method of avoiding pregnancy.
- Natural methods of contraception involve the pull-out method, calendar method, lactational amenorrhea, and cervical mucus method.
- Different contraceptives have varying advantages, drawbacks, and success rates.
- It is essential to consult with a healthcare expert to determine the best method for an individual’s requirements and circumstances.
Considerations For Pregnancy Prevention Methods
The suitable pregnancy prevention method or contraception could vary based on various factors, including the following.
- Experience with previous contraceptive methods, including success and failure rates and side effects
- Yours and your partner’s age and general health, including any history of sexually transmitted diseases (STDs)
- Frequency of intercourse
- Plans for future pregnancies
- Your and your partner’s comfort using a specific contraceptive method and any privacy concerns
Not all aspects may apply to all women, and some may have exclusive factors. You may consult your doctor to determine the best pregnancy prevention method for your case (38).
Hormonal Ways To Prevent Pregnancy
Pregnancy can be avoided using hormonal contraceptives. These are medications or implants that release synthetic hormones to prevent ovulation. They also thicken the cervical mucus, making it difficult for the sperm to reach the egg cell (2).
All hormonal contraceptives, except emergency contraceptive pills, require a doctor’s prescription.
Hormonal contraceptives to prevent pregnancy include:
1. Implants
These are tiny hormone-releasing devices implanted under the skin of the woman’s upper arm.
Norplant (6 implants), Jadelle (2 implants), and Nexplanon (formerly Implanon; 1 implant) are some common brands of hormonal implants. These implants release etonogestrel or desogestrel hormones that suppress ovulation. Currently, nexplanon is the worldwide available brand as it consists of only a single implant (compared to Norplant and Jadelle). Thus, it is easier to place and remove.
- They start to prevent pregnancy within 24 hours upon insertion within the first week of the menstrual cycle.
- If implanted after five days of the menstrual period, you should use contraception for up to seven days to prevent pregnancy (or abstain from intercourse). If intercourse occurs within these first five days, an emergency contraception is indicated.
An implant generally works for three years, and you can remove and place a new implant on the same day if you would like to continue with hormonal contraception
. It has only a 0.01% failure rate in three years, if appropriately inserted, making it the most effective form of hormonal contraception (1) (3).
 Quick fact
Quick fact2. Birth control patches
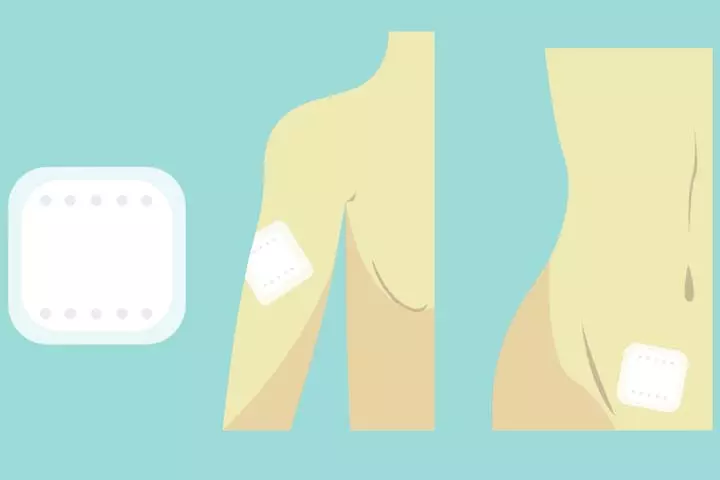
Birth control patches (also called combination patches, transdermal patches, or skin patches) prevent pregnancy by releasing estrogen and progesteroneiA female reproductive hormone that plays an essential role in menstruation, pregnancy, and breastfeeding. into the bloodstream; thus suppressing ovulation and changing the consistency of cervical mucus.
It is recommended that you use the patch for 21 days to avoid pregnancy. Patches are replaced once a week for three weeks, and it is advised to change the location of the patch to prevent skin irritation.
You may have to check the patch to make sure that it is in place. It can be placed on the underarm, abdomen, or buttocks. It has a failure rate of 7% with typical use (less than 1% with perfect use) (1) (4).
3. Contraceptive injections
Also called contraceptive shots, contraceptive injections release hormone progestin to your bloodstream and suppress ovulation to prevent pregnancy. These are available under the brand names Depo-Provera, Sayana Press, or Noristerat.
- Depo-Provera and Sayana Press give you protection from pregnancy for up to 13 weeks, whereas Noristerat protects you from pregnancy for up to eight weeks.
- Contraceptive injections are immediately effective if taken within the first five days of the menstrual cycle.
- If you received an injection after five days of the menstrual cycle, you have to use contraception for seven days to avoid pregnancy (or abstain from intercourse). If intercourse occurs within these first five days, an emergency contraception is indicated.
- Injections can be chosen as a way to prevent pregnancy after a loss or termination of pregnancy, or after childbirth. This method, as with any hormonal contraception that contains progestins without estrogeniA hormone responsible for the development and functioning of female reproductive organs. , can start immediately after any of these events.
It is a highly effective method of contraception with a failure rate of just 0.3% (1) (5) .
4. Hormonal vaginal contraceptive rings
The small, flexible plastic rings can be placed in your intimate area to avoid pregnancy. They release synthetic estrogen and progestin hormones to the bloodstream. They suppress ovulation, and you may observe changes in the thickness of cervical mucus.
Nuvaring is one of the famous brands. It can be used for three weeks and has a 7% failure rate with typical use (1) (6) .
The hormonal contraceptive rings may cause headaches and irritation in the intimate part or discharge in some women.
5. Progestin-only oral contraceptives
Also called mini-pills, progestin-only oral contraceptives are recommended for lactating mothers and women with contraindications to estrogen use. Norgestrel, Norethindrone, and Drospirenone are the different formulations of mini pills. These tablets suppress ovulation and thicken cervical mucus.
- You may start taking them from the fifth day of your menstrual cycle and on a daily basis.
- If you miss a pill, take it as soon as you remember, and continue to maintain the same schedule from the next day.
- If the tablet is taken more than three hours from the scheduled time, you should use backup contraception for the next 48 hours to avoid pregnancy. If you are using pills containing Drospirenone, a backup method is indicated if the pill is taken more than 12 hours.
These pills are 99% effective if taken on schedule. However, if you miss pills, the effectiveness falls to 91%.
Women can return to fertility immediately after discontinuation of this pill. It may cause adverse effects such as nausea, tenderness in busts, headache, or menstrual irregularities (7) (8).
6. Combination oral contraceptives
Combination oral contraceptives contain synthetic estrogen and progesterone hormone. These pills are effective if taken regularly at a scheduled time and have a 7% failure rate with typical use (1).
Combination oral contraceptives are classified into three groups (9):
- Monophasic 21-day pills: These are the most common type. They are taken for 21 days, followed by a seven-day break. All the pills contain the same amount of hormone. Microgynon, Marvelon, Yasmine, and Cilest are some of the popular brands of monophasic tablets.
- Phasic 21-day pills: These are taken for 21 days, followed by no pills for seven days. They contain different amounts of hormones, come in different colors, and should be taken in a prescribed order. Logynon is one of the popular phasic pill brands.
- Every day (ED) pills: These come in a pack of 21 hormonal pills and seven placebo (inactive) tablets. The pills should be taken every day in the prescribed order. Microgynon ED is a popular brand of ED pills.
7. 91-day combination oral contraceptives
These birth control pills contain estrogen and progesterone. These hormonal pills are for 12 weeks and seven estrogen-only (hormone-free) pills for the last week. Seasonale is a popular brand of 91-day combination pills (10).
Hormonal ways to prevent pregnancy may not be recommended for obese women, smokers, women who are older than 35 years, and women with a history of blood clots. These are also not recommended for women who experience (11):
- Unexplained uterine bleeding
- Significant liver disease
- Breast or uterine cancer
Side effects:
These contraceptives may cause headaches, acne, hair loss, nausea, painful menstruation, increased risk of blood clots, or breast pain in a few women (39).
Advantages of hormonal methods: These have higher efficacy compared to other methods. You can go back to fertility after discontinuing hormonal contraceptives.
Disadvantages of hormonal methods: Hormonal implants do not protect you from sexually transmitted diseases.
Emergency Contraception

Emergency contraception, also known as emergency postcoital contraception, is the use of a drug or device to avoid pregnancy after unprotected intercourse. Taking an emergency contraceptive pill within 72 hours can help prevent pregnancy.
Emergency contraceptives include (12):
- Copper T380 intrauterine device: It can be placed up to seven days after unprotected intercourse to prevent pregnancy.
- Progesterone-only emergency contraception: The progestin levonorgestrel tablet is most effective in the first 72 hours and can be taken up to 120 hours after unprotected intercourse.
- Progesterone agonist/antagonist: Available under the name ulipristal, it should be used 120 hours after unprotected intercourse. In case you vomit within three hours after taking a tablet, you have to take one more.
- Combined hormone emergency contraception: Also known as the Yuzpe regimen, it involves the use of ethinyl estradiol and levonorgestrel at a higher dose compared to regular contraception.
Ella or Ellaone is a non-hormonal, morning-after pill, containing 30mg of ulipristal acetate. It is an effective pill to avoid pregnancy after unprotected intercourse. You may require a prescription to buy this pill. However, according to the American College of Obstetricians and Gynecologists, a copper intrauterine device (IUD) is the most effective form of emergency contraception (13). It has a failure rate of only 0.09%.
The adverse effects of emergency contraceptive pills include:
- Nausea
- Vomiting
- Minor changes in menses
- Breast tenderness
- Fatigue
- Headache
- Abdominal pain
Disadvantages:
Emergency contraceptives do not protect you from STDs.
Note: Emergency contraception may be used more than once in the same cycle if indicated. However, it is not a regular method of contraception and should not be used continuously because it is significantly less efficient than regular contraception. You may consider other methods of contraception with the guidance of your physician (14).
Intrauterine Devices To Prevent Pregnancy
The use of an intrauterine device (IUD) is one of the most effective methods to prevent pregnancy. An IUD can be a copper-releasing or hormone-releasing type (15):
- A copper-releasing IUD is a T-shaped device that damages the sperm and reduces its motility to prevent fertilization. It can prevent pregnancy for up to 12 years.
- Mirena, Liletta, Skyla, and Kyleena are intrauterine hormonal devices that contain levonorgestrel to prevent pregnancy.
You shouldn’t use IUDs in the following cases:
- Abnormalities of the uterine cavity
- Genital bleeding of unknown cause
- Uterine or cervical cancers
- Wilson diseaseiA rare genetic disorder wherein excess copper builds up in the body, causing damage to the vital body organs. (for copper-containing IUDs)
- Pregnancy
- Cervical infections
- Endometrial infections.
IUDs produce no adverse systemic effects, and their advantages are:
- Reduced ectopic pregnanciesiA medical condition where the fertilized egg implants outside the female uterus, usually in the fallopian tubes.
- Decreased menstrual blood loss and dysmenorrheaiPainful menstruation often caused due to medical reasons such as uterine fibroids or endometriosis.
- Decrease in risks of pelvic inflammatory disease
- Decrease in risks of synchronous endometrial and ovarian canceriA rare condition identified by the presence of both endometrial and ovarian cancers simultaneously in a female. (SEOC)
Disadvantages of IUDs:
The insertion of IUDs is associated with a potential risk of uterine perforation in a small percentage and the accidental removal or displacement of IUD within three months of insertion (15). They do not protect against STDs.
 Quick fact
Quick factBarrier Ways To Prevent Pregnancy
Barrier methods of contraception prevent the sperm from coming into contact with the ovum. Mechanical barriers prevent direct contact, and chemical barriers destroy the sperm.
Learn how to avoid pregnancy using barrier methods:
14. Male contraceptive
A male contraceptive is a thin latex or polyurethane sheath that is placed over the male private part to prevent the passage of male reproductive fluid to the female intimate region.
- Male condoms have a 13% chance of failure rate (1).
- They are easily available and cost-effective.
- They help prevent unintentional pregnancy and STDs (16).
In rare cases, contraceptives may fail to prevent pregnancy. Inappropriate use of contraceptives may result in pregnancy. Read the manufacturer’s instructions, and always check the expiry date of contraceptives before using them.
15. Female contraceptive
A female contraceptive is made of polyurethane sheath. It can be placed in the birth canal for birth control.
- It acts as a barrier to help prevent contact of male reproductive fluid with the birth canal.
- It is not recommended to use both female and male contraceptives at the same time as it may lead to damage or displacement of the contraceptives.
- It has a 21% failure rate (1).
- It may help to prevent STDs.
- It can be inserted eight hours before intercourse. However, if you wear the contraceptive for a prolonged period, you may end up having a urinary tract infection (17).
16. Diaphragm

A diaphragm is a shallow latex cup that can be placed in the intimate area to act as a barrier to prevent pregnancy.
- It can be placed before intercourse, as it is free of hormones.
- Spermicide is applied to the inside of its dome.
- The diaphragm provides protection for up to a few hours if you use the exact size.
- You should wait a minimum of six hours after lovemaking to remove the diaphragm.
- A diaphragm has a 17% failure rate in typical use (1).
A diaphragm may cause urinary tract infections if used for a long duration. It does not protect you from STDs (18).
17. Cervical cap
A cervical cap is placed above the base of the cervix to prevent pregnancy. It is advised to fill one-third of the cap with spermicide before insertion. It can be inserted eight hours before intercourse and can be left in the cervix for up to 48 hours.
- It acts as a mechanical and chemical barrier when used with spermicide.
- It has a 17% failure rate (1).
- The cervical cap provides contraception until its duration of use.
- It may cause cervical erosioniCondition where cells from inside the cervix develop outside it, causing vaginal bleeding and inflammation. and uterine bleeding.
- It is not recommended for women who have positive PAP test results, and a high failure rate is seen in obese women due to displacement.
- Placing it more than 48 hours inside your body can result in toxic shock syndromeiA rare complication of a bacterial infection where harmful toxins are released in the bloodstream, affecting multiple organs of the body. .
Cervical cap is 86% effective in preventing pregnancy for those who have not given bith, but only 71% effective for women who have given birth before. It does not prevent STDs as well (19).
18. Contraceptive sponge
It is a soft, disk-shaped polyurethane device containing spermicide. It kills sperm and prevents pregnancy if placed deep in the female intimate part. It can be placed 24 hours before intercourse.
- It is recommended to remove the sponge at least six hours after intercourse. The sponge may cause infection if you keep it for more than 24 hours in the female intimate region .
- It does not protect you from STIs.
It has a 14% failure rate among women who have never been pregnant and a 27% failure rate in women who have had a baby (1) (20).
19. Spermicidal agents
These are chemical barriers containing surfactants that damage the sperm cell membrane. They should be applied to the intimate region in advance to avoid pregnancy.
These are available as:
- Spermicides
- Suppositories
- Jellies
- Films
- Foaming tablets
- Creams
The chemical, spermicide, may destroy bacteria and viruses, thus decreasing the risk of infections. However, clinical data are limited regarding the efficacy of spermicide in the prevention of HIV.
These may destroy normal bacteria in the flora present in the intimate area. Escherichia coliiA bacteria that typically colonizes the human intestines, a few strains of which may cause harmful diseases. colonization is shown to increase after the use of spermicide and may lead to urinary tract infections in a few women. They have a 21% chance of failure rate (1) (20).
Advantages of barrier contraceptives: They are easily available and inexpensive. They can be used by breastfeeding mothers or anyone with health problems such as hypertension.
Disadvantages of barrier contraceptives: They may cause interruption during intercourse. They have a higher failure rate than hormonal methods.
Permanent Ways To Prevent Pregnancy
Sterilization is an effective and permanent way to avoid pregnancy. It is a surgical technique to prevent fertilization. It can be done for both women and men.
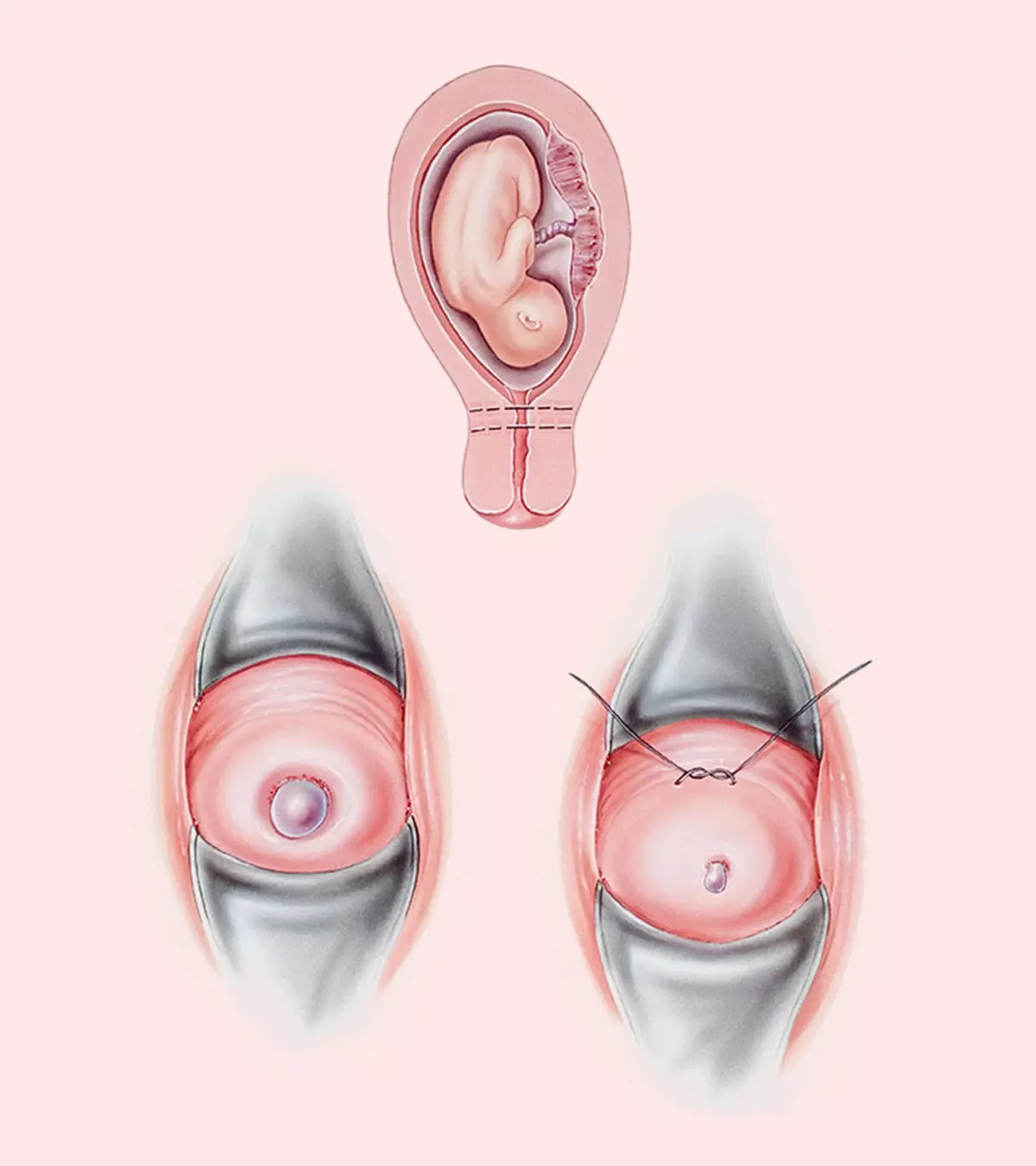
20. Female sterilization
Female sterilization is achieved by surgery, the ligation of fallopian tubesiTube-like structures connecting the ovaries and uterus that help transport eggs for the fertilization process. , or rarely, if required, due to other reasons by hysterectomy (removal of the uterus). The fallopian tube is cut, sealed, clipped, and tied on each side to prevent fertilization (21).
The Essure system is a permanent birth control for females. The sterilization process involves placing small metal and fiber coils in the fallopian tubes to create scar tissue in the fallopian tube and prevent fertilization (22). However, the option has become limited due to some after-placement concerns and the product is no longer manufactured.
It has a failure rate of 0.5% (1).
21. Male sterilization
Vasectomy
is a permanent way of sterilization for males. In this method, the vas deferens are ligated or fulgurated (destroy the growth of tissue with diathermyiA technique where controlled heat (from electric currents) is passed beneath the skin to relieve pain and destroy abnormal tissues. ). This procedure prevents sperm from reaching the urethra.
Hematoma, infection, and sperm granulomas are possible complications of the male sterilization procedure. There is a 0.15% chance of failure in this procedure (1).
Advantages of sterilization: It does not involve hormones, and there is no evidence indicating any effects on the libido, menstrual cycle, or lactation.
Disadvantages of sterilization: It does not prevent you from contracting STDs (21).
 Research finds
Research findsNatural Methods Of Contraception
These are the most common ways of preventing pregnancy. If your religious and cultural beliefs do not allow the use of medications or devices for contraception, you could opt for these methods. Avoiding intercourse during your fertile period could also help prevent pregnancy.
However, the failure to determine the exact fertile period and mistakes in withdrawal methods could lead to pregnancy. Natural methods of contraception have a high rate of failure, and it is recommended to follow other techniques. None of these methods protect you from STDs.
Natural Contraception Methods Include:
22. Coitus interruptus
Also known as withdrawal or pull out method, it involves the withdrawal of the male private part from the female intimate area before ejaculation. Its efficacy depends on a man’s capability to withdraw prior to ejaculation. It has a 4% failure rate (23).
23. Lactational amenorrhea
It is the temporary absence of menstruation after childbirth. This occurs due to the increased levels of prolactin, which is a hormone that triggers milk secretion in mothers. These hormones suppress ovulation in breastfeeding women.
This type of contraception is best observed when you breastfeed your baby every four hours during the day and every six hours at night (24).
24. Calendar method
It is also known as the rhythm method. This method is based on the following facts:
- An egg lives for only 24 hours after ovulation.
- Sperm is viable only for 48 hours after intercourse.
- Ovulation occurs between 12–16 days of a cycle.
Fertility awareness is useful for predicting ovulation and identifying the fertile window. The fertility period is determined based on the menstruation dates for six months. Subtracting the number of days in the shortest menstrual cycle by 18 will give you the earliest day of fertility period. Subtracting the number of days in the most extended cycle by 11 will provide you with the latest day of the fertile period (25).
Tyiece Aveley, a blogger, shares her experience with the calendar method as a form of birth control. She says, “I’ve been using the calendar method for the past six or seven years, and I’ve never gotten pregnant while using it (i).” Additionally, she recommends using a mobile app to simplify the tracking of menstrual cycles and ovulation.
25. Cervical mucus method
The fertility period can be predicted by quantifying the cervical mucus with fingers. Mucus usually becomes more elastic and copious during these days due to increased estrogen hormone in your body.
You may be able to understand the increased amount of cervical discharge during these days. The safe period for intercourse begins four days after maximal cervical mucus and continues until the onset of the next menstruation (26).
26. Basal body temperature method
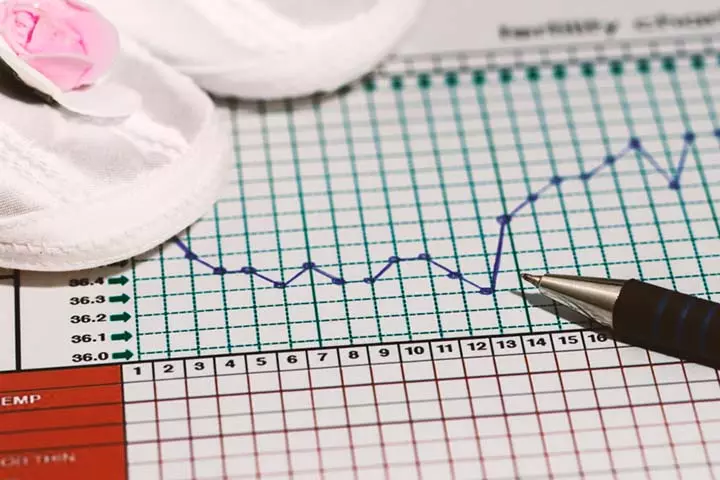
The measurement of basal body temperature (BBT), that is, your body temperature while you are at rest, will help you to recognize the end of the fertility period in a cycle. The calendar method or cervical mucus method is used to determine the first day of the fertile period. There can be a slight increase in basal body temperature after ovulation, ranging from 0.5ºF/0.3ºC to 1.0°F/0.6ºC (27).
Basal body temperature may vary due to the following factors (28):
- Fever
- Diseases
- Stress
- Change in work schedules
- Changes in sleeping time
- Alcohol consumption
- Travel
- Gynecological disorders
- Certain medication
27. Symptothermal method
This technique is based on self-assessment of the basal body temperature and thickness of cervical mucus. Biological changes of the cervix may not be evident in some women during the fertile period (27).
Advantages of natural methods: These are preferred as they involve no devices, no cost, and no chemicals. These are viable options if a couple’s religious and cultural beliefs do not permit the use of medications or devices for contraception. Moreover, these methods have no adverse effects.
Disadvantages of natural methods:The chance of unintentional pregnancy is high, and they do not prevent STDs. Natural ways of contraception are not suitable if you have irregular and unpredictable cycles.
A 2–23% failure rate is noted in the typical use of these methods (1).
Prevalence of Contraceptive Use
According to the World Health Organization, the number of women desiring modern methods of contraception has witnessed a global increase. Over a period of two decades between 2000 and 2025, the prevalence rate for the use of contraception among women of reproductive age has increased from 73.6% to 76.8%.
Studies done on the US population between 2017-19 by the Centers for Disease Control and Prevention have indicated that 65.3% of women aged between 15 and 49 years currently use contraception. The most preferred and common contraceptive methods were female sterilization (18.1%), oral contraceptives (14%), long-acting reversible contraceptives or LARCs (10.4%), and male condoms (8.4%). However, with education, the preference for pills in place of sterilization procedures is increasing among the younger population.
However, earlier studies also showed that women rely more on female sterilization to prevent pregnancy as they age. For those aged 40-49, almost 40% use this method. Younger women, mainly those aged 15-19, prefer using the pill. Condom use is less common among all age groups except 20-29. Younger women use long-lasting contraceptives more than older ones, except for women aged 30 to 39, who also use them a lot. Women aged 40 to 49 use them the least.

Contraceptive use among US women by age group (2015-2017)
Source: Current Contraceptive Status Among Women Aged 15–49: United States, 2015–2017; CDCFrequently Asked Questions
1. Can you get pregnant if you forget to take the pill one day?
If you miss one pill on your daily pill regime, it may not cause pregnancy. You should take the missed pill as soon as you remember, even if it means you should take two pills in a day. There is no requirement for additional contraception. You may continue your daily pill on time.
If you miss taking the pill for two days or more, it may result in pregnancy. In such cases, you should use contraception for the next seven days (29).
2. Can birth control pills cause infertility in the future?
Birth control pills may not cause infertility. Usually, irregular menstruation, ovulation problems, infections, and implantation failure may cause infertility in females (30). Infertility may also be caused by male factors such as sperm count and sperm motility.
Women return to fertility after the discontinuation of birth control methods. There is no scientific evidence from randomized control trials indicating infertility or birth defects in fetuses caused by birth control methods (31).
It is recommended to seek your doctor’s help to choose appropriate birth control methods, depending on your conveniences and requirements.
3. At What age should you stop taking birth control pills?
According to the American College of Obstetricians and Gynecologists and the North American Menopause Society, women should continue using contraceptives until menopause or age 50 to 55 years (34).
4. How can vinegar prevent pregnancy?
Vinegar does not prevent pregnancy. Further, if applied in the vagina, it causes an imbalance in natural bacterial balance that may increase the risk of vaginal infections (35).
5. Does water and salt prevent pregnancy?
No, salt and water are not effective in preventing pregnancy (36).
6. Can hot drinks prevent pregnancy?
No, drinking hot water or hot drinks is not a contraceptive measure (37).
You may avoid pregnancy with the help of various pregnancy prevention methods such as oral contraceptives, birth control patches, contraceptive shots, and intrauterine devices (IUD). If these methods aren’t suitable for you, you may try natural ways such as the basal body temperature method (BBT) or calendar tracking methods to prevent pregnancies. However, do not rely on food-related and other misconceptions, such as douching, to avoid pregnancy. Instead, you may talk to a health professional to understand the best-suited method to prevent pregnancy safely.
Infographic: Things You Must Be Mindful Of When Using Contraceptives
Preventing pregnancy is possible with different contraceptive methods available today. But, there are still many cases of unplanned pregnancies worldwide, even with the use of contraceptives. One of the most common reasons for these occurrences is the incorrect use of birth control measures. Take a look at the infographic below to learn about some common mistakes when using contraceptives. Illustration: Momjunction Design Team
Learn about the different female birth control options available to help you plan your family. Get informed on the pros and cons of each option.
Personal Experience: Source
MomJunction articles include first-hand experiences to provide you with better insights through real-life narratives. Here are the sources of personal accounts referenced in this article.
i. How I use natural family planning to prevent pregnancy;https://www.youtube.com/watch?feature=shared&v=lCsuefLt9eA
References
Community Experiences
Join the conversation and become a part of our nurturing community! Share your stories, experiences, and insights to connect with fellow parents.
Read full bio of Dr. Sherif Abdelkarim Mohammed Shazly
Read full bio of Dr Bisny T. Joseph
Read full bio of Rebecca Malachi
Read full bio of Aneesha Amonz