Image: iStock

Melanoma (malignant tumor) is a type of skin cancer where melanocytes grow out of control. Melanocytes are skin cells that produce melanin, a pigment imparting color to one’s hair, skin, and eyes. According to the National Institute of Health (NIH), although rare, melanoma is the third most common skin cancer type in children, commonly affecting teens between 15 and 19 years (1).
Generally, melanoma can develop anywhere on the skin (epidermis), but it can also occur in the eye (2). Medically, melanoma is considered the most dangerous skin cancer type because it can rapidly spread to other body parts, including vital organs (3). Hence, timely detection and prompt treatment of melanoma in children are crucial.
Keep reading while we tell you about the types, signs and symptoms, possible causes, diagnosis, and treatment of melanoma in children.
Key Pointers
- Melanoma is divided into three types and can occur due to factors such as genetics, recurring exposure to X-rays, and immunodeficiency.
- The first indication of melanoma in children is the appearance of a mole and its progressive changes.
- A physical examination based on the dermatologist’s ABCDE rule can help diagnose the condition.
Types Of Melanoma
Melanomas are of three different types (2).
- Conventional melanoma (CM): CM, also known as adult-type melanoma, is the melanoma type that has causes and risk factors similar to those for adults.
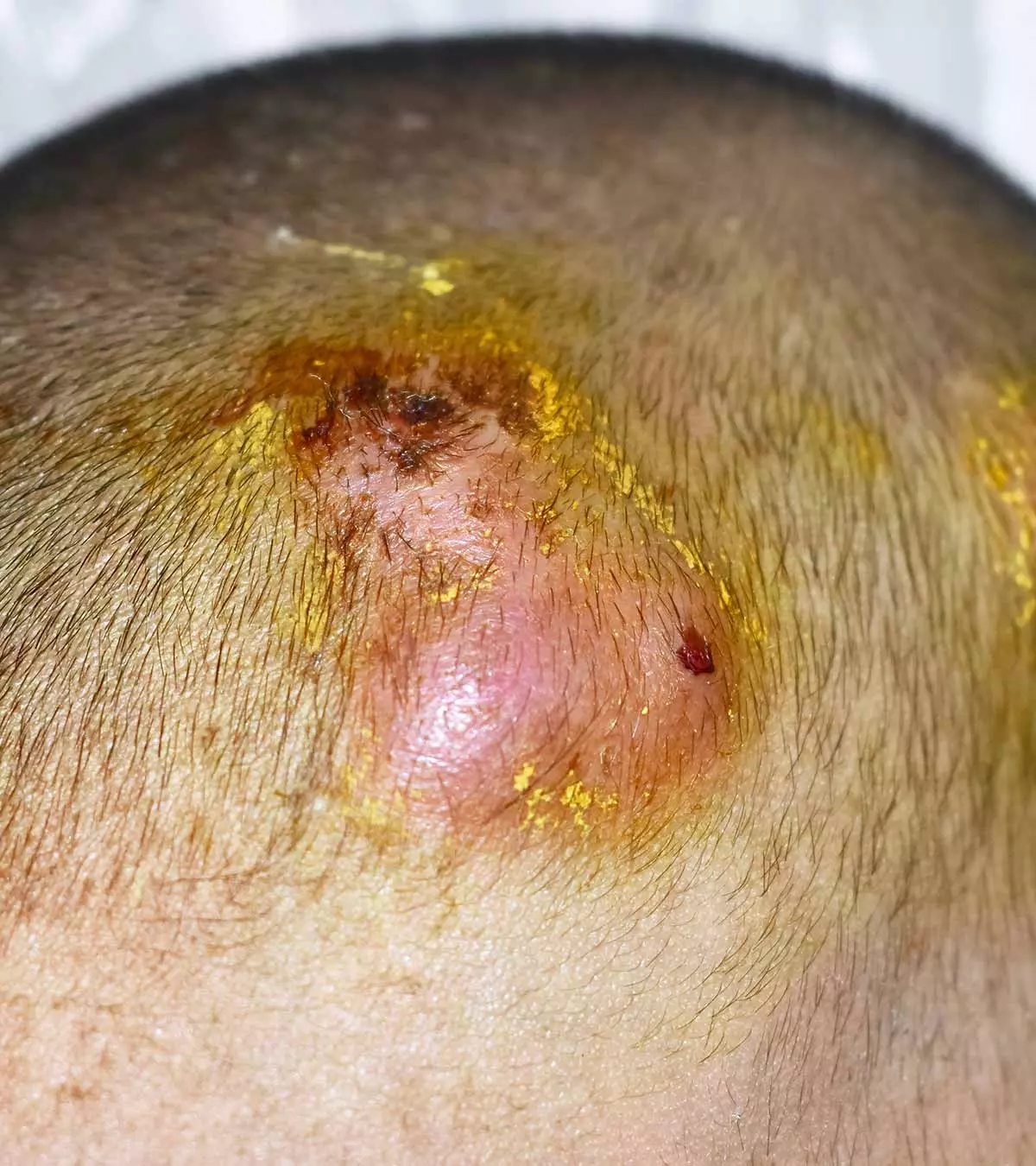
- Spitzoid melanoma (SM): It’s the most common melanoma type in children, often appearing as a cluster of tissue that the child can feel under the skin. This cluster of tissue is usually round, has one color, and is found on the head, hands, or legs.
- Congenital melanocytic nevus (CMN): It’s a type of melanoma that develops from a large, pigmented congenital mole (spitz nevus) or birthmark.
Identifying the exact melanoma type is crucial to ensure proper testing, treatment, and prognosis of the disease, but this is normally done by a health professional.
Signs And Symptoms Of Melanoma
Most melanomas don’t cause any specific symptoms in the early stages. However, as the disease progresses, signs and symptoms could appear. The most common sign of melanoma is the change in color, shape, size, and feel of a mole. So, parents and caregivers should keep an eye on a mole or growth that (2) (4) (5):
- Changes or grows fast
- Has an odd shape or is large
- Feels bumpy to touch and sticks out from the surrounding skin
- Has whitish, yellowish, pink color, or no color
- Has more than one color
- Itches, pains, or forms a scab and bleeds
- Looks like a sore that doesn’t go away
Besides these, the appearance of a dark spot under a toenail/fingernail that’s not caused by an injury or trauma to the nail should also be checked. Do note that most moles aren’t melanoma, and their appearance is often common in children until puberty (4).
Causes Of Melanoma In Children
The precise reason why children develop melanoma is unknown. But, certain risk factors are known to raise a child’s chance of developing childhood cancer or melanoma (2).
- Family history of melanoma
- Fair skin, light-colored hair, blue eyes, and freckles
- Many small moles or several large moles on the skin
- History of blistering sunburns
- Chronic or frequent exposure to X-rays
- ImmunodeficiencyiA condition where the body’s immune system function is disrupted due to various factors, making one prone to diseases and infections. or immunosuppressioniReduction in the functional abilities of the immune system due to a medical condition or medication.
- History of retinoblastoma (eye cancer type that starts in the retina)
- Certain congenital conditions, such as xeroderma pigmentosumiAn uncommon genetic condition where the skin becomes extremely sensitive to UV radiation, increasing the risk of cancer. , Werner syndromeiRare genetic disorder causing rapid aging, often occurring after puberty. , and melanocytic neviiAccumulation of melanocytes (pigment-producing skin cells), causing benign dark patches on the skin.
 Point to consider
Point to considerDiagnosis Of Melanoma In Children
After collecting the child’s medical history and noting their risk factors, a pediatric oncology specialist performs the following tests to diagnose melanoma in children (6).
1. Physical examination
In this test, the doctor examines the mole (or any abnormal spot on the skin) using the ABCDE rule developed by dermatologists. The ABCDE rule checks different features of a mole. If one or more of the features show progression, increase, or change, it could be considered a red flag.
A – Asymmetry
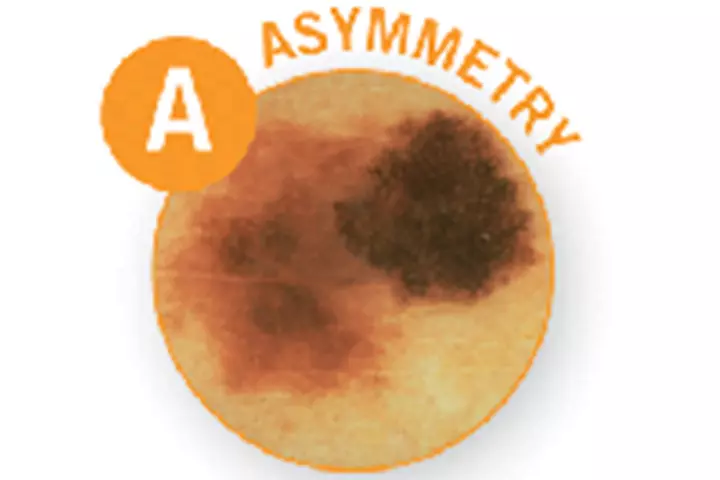
B – Border

C – Color
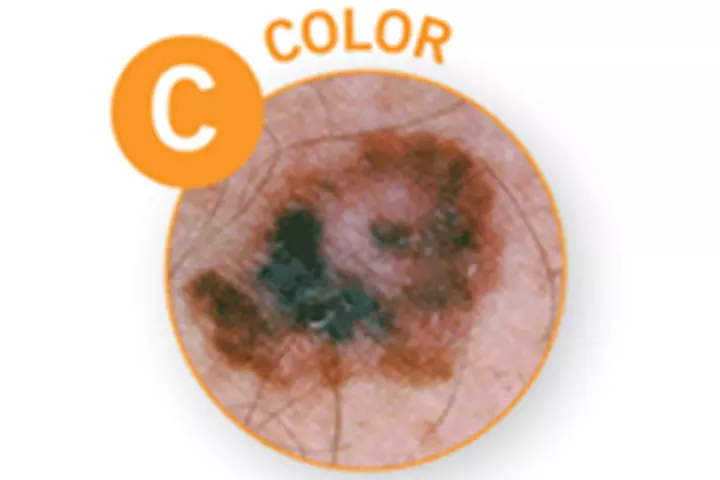
D – Diameter

E – Evolving
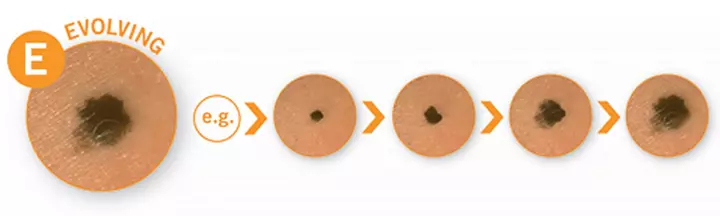
Generally, melanomas in children are almost the same as melanoma in adults. However, doctors follow the ABCDE rule with additional detection criteria in children aged ten years and younger. For instance, melanoma in children usually has one color, which may not be black or brown. Likewise, melanomas tend to be flatter in adults, whereas they often appear like a firm, raised bump in children (5).
2. Biopsy
If a doctor suspects a melanoma, they will remove the affected area and send it to a specialized laboratory to see if the cells are cancerous. In addition, they will also see how deep the cancer cells are in the skin to determine the risk of melanoma spreading.
The graph below illustrates the annual incidence of melanoma cases in the US population between 2018 and 2025. The data shows that the number of melanoma cases reported during the mentioned period has increased. However, the fatalities have decreased considerably, indicating an improvement in the disease’s mortality rate, which could be attributed to timely diagnosis and treatment initiation.

Melanoma statistics in the US population (2018-2025)
Source: Dermatoscopic image melanoma recognition based on CFLDnet fusion network; Multimedia Tools and ApplicationsTreatment For Melanoma In Children
The treatment for melanoma depends on its stage (stage 0, 1, 2, 3, 4). As the stage progresses, the treatment course varies. (2) (6).
- Surgery: Surgery removes the entirety of the melanoma and some of the normal surrounding tissue. If a nearby lymph node also has cancerous growth, it’s also removed. This is done to cease the spread of cancerous cells to other areas and body parts. Some melanomas may require more invasive and extensive surgical procedures than others.
- Chemotherapy: This treatment modality may be initiated when cancer has spread to nearby lymph nodes or other organs. A child can be given medications via mouth, injection, or intravenous fluid (IV). The medicine is given to kill cancer cells or prevent their multiplication. In some cases, more than one chemo (combination chemo) may be used. High-energy radiation (radiation therapy): Specifica radiation beams are focused on a specific area to kill the cancer cells and prevent further spread.
- Immunotherapy: Immunotherapy (biologic therapy) is the treatment method wherein a person is given a substance that stimulates an immune response. These substances sensitize the child’s immune system and train them to detect and destroy cancer cells. This therapy may be used for children 12 years and older for whom surgical removal of melanoma isn’t possible.
- Targeted therapy: This treatment method involves using certain medications that directly work on the cells that carry mutated genes that trigger melanoma. For instance, BRAF and MEK inhibitors are medications that target cells with BRAF gene mutation.
Early detection and treatment of melanoma raise a child’s five-year survival by more than 90 percent. The survival rate is 70 percent if the melanoma has spread only to the nearby lymph nodes. However, if melanoma spreads to other blood vessels and body parts, the five-year survival rate is 25 percent.
 Did you know?
Did you know?Possible Complications Of Melanoma Treatment
Here’s a brief list of side effects and complications a child may experience due to different melanoma treatment options (7).
- Localized damage to the healthy surrounding skin
- Swelling, reddening, or blistering of the skin around the operated area
- Pain or itching on the operated area
- Scarring or skin color change after skin removal
- Secondary infection at the surgery site
- Bleeding during and after surgery
- Reaction to medication or drug-drug interactions
- Recurrence after treatment, especially at a distant site (metastatic melanoma)
Besides these, if a child’s lymph nodes have been removed, they may develop swelling on the neck, arm, or leg due to fluid retention (lymphoedema).
Prevention Of Melanoma In Children
Knowing the risk factors associated with melanoma and keeping a close watch on children may help with a timely detection of the disease. Here’s what you can do (8).
- Monitor your child’s skin: Follow the ABCDE rule and look for the shape, size, and color of any mole or spot. If a child has one or more risk factors for melanoma, a dermatologist must examine them annually. Melanomas don’t necessarily occur in places exposed to the sun. Check the skin on body parts not usually exposed to the sun as well, such as the palms and soles.
- Keep your child away from direct sun: Generally, sun exposure (UV rays) is the main cause of melanoma in adults, but this isn’t the case in children (2). Despite this, it is highly advised that children wear sunscreen before stepping out in the sun. Choose a sunscreen with SPF 30 or higher and avoid exposure to the midday sun between 10 am and 4 pm. Dress your child in protective clothing, such as a hat and shirt. Since melanoma can occur in the eye, ensure your child wears sunglasses while in the sun.
 Quick tip
Quick tip- Using tanning beds before 18 years of age raises a child’s risk of developing melanoma by 85 percent (6).
Frequently Asked Questions
1. Is melanoma in children curable?
If detected early, melanoma present on the skin surface can be cured. However, if melanoma progresses and travels under the skin to the blood vessels, the lymphatic system, and nearby organs, such as the lungs and brain, it often becomes incurable (9) (10).
2. How serious is melanoma in children?
Melanoma in children is one of the most serious and rare skin cancers. Every year, around 300 to 400 cases are reported in the US. However, due to its rarity, it often goes undiagnosed until later stages (5).
3. What are some common myths and misconceptions about melanoma in children, and how can these be addressed?
Some common myths and misconceptions concerning cancers like melanoma are that it is contagious, cancer gets worse with the more sugar you consume, and that cancer is mostly fatal. However, all of these myths are not true. The chances of survival with cancer have improved by over 90% from what it was in the 1990s due to technological advances; even though cancer cells consume more glucose/sugar than normal cells, there is no correlation with the consumption of more sugar. Finally, cancer is not contagious except in the rare instance that cancerous tissue is transplanted into a healthy host (11).
4. What are the different stages of melanoma, and how does treatment vary depending on the stage of the disease?
There are four stages of melanoma based on its progression. Stage 0 is the initial stage, where the cancer is only found in the skin’s top layer and can be treated and removed with surgery. Stages I and II often necessitate wide excision surgery; in both cases, cancer has not yet reached the lymph nodes. In stage III, cancer spreads to the nearby lymph nodes and is treated through wide excision of the primary tumor along with lymph node dissection. The IVth and final stage is when cancer has metastasized to other parts of the body and may be treated by surgery or radiation therapy (12).
5. How often should children be screened for melanoma?
Children with a family history of the disease should get an annual total body skin exam by a healthcare provider. Besides, they should conduct a skin exam by themselves on a monthly basis. Regular skin exams, both professional and self-exams, are important for early detection of melanoma.
A child’s skin health is important for every parent. Melanoma in children is a fatal form of cancer and requires immediate treatment upon detection. But this can be tricky since early signs may not be possible to detect. Hence, a child with risk factors such as a family history of melanoma, immunodeficiency, and congenital conditionsiStructural or functional abnormalities present from birth in an individual. must be checked. Early detection and treatment are the keys to a good survival rate. Remember, any form of cancer, such as melanoma, requires utmost care and support from family. So don’t lose hope, help the children stay strong, and be regular with the treatments.
Infographic: Caring For Your Child’s Skin During Radiation Therapy For Melanoma
The radiation therapy to treat melanoma may cause side effects on the skin. However, following the proper skincare routine can help minimize these side effects and boost recovery. Go through this infographic to learn some skincare tips for children undergoing radiation therapy.
Some thing wrong with infographic shortcode. please verify shortcode syntax
Illustration: Melanoma In Children: Symptoms Diagnosis And Treatment

Image: Dall·E/MomJunction Design Team
Watch this video where the doctor discusses the diagnosis and treatment of pediatric melanoma. Learn about the latest research and best practices for this serious condition.
References
- Childhood Melanoma Treatment (PDQ®)–Patient Version.
https://www.cancer.gov/types/skin/patient/child-melanoma-treatment-pdq#_720 - Melanoma.
https://www.stjude.org/disease/melanoma.html - Skin Cancer Basics.
https://www.cdc.gov/skin-cancer/about/index.html - Pediatric Melanoma.
https://www.aimatmelanoma.org/melanoma-101/types-of-melanoma/pediatric-melanoma/ - Melanoma Can Look Different In Children.
https://www.aad.org/public/diseases/skin-cancer/types/common/melanoma/different-children - Childhood Melanoma.
https://www.dana-farber.org/childhood-melanoma/ - Skin Cancer in Children.
https://www.urmc.rochester.edu/encyclopedia/content.aspx?ContentTypeID=90&ContentID=P01922 - Protect your kids from skin cancer.
https://www.mdanderson.org/publications/focused-on-health/protect-kids-from-skin-cancer.h29-1591413.html - Melanoma.
https://kidshealth.org/en/parents/melanoma.html - Melanoma Cells Are More Likely to Spread after a Stopover in Lymph Nodes.
https://www.cancer.gov/news-events/cancer-currents-blog/2025/melanoma-spread-lymph-nodes-ferroptosis# - Common Cancer Myths and Misconceptions.
https://www.cancer.gov/about-cancer/causes-prevention/risk/myths - Treatment of Melanoma by Stage.
https://www.cancer.org/cancer/types/melanoma-skin-cancer/treating/by-stage.html
Community Experiences
Join the conversation and become a part of our nurturing community! Share your stories, experiences, and insights to connect with fellow parents.
Read full bio of Dr. Jaime Fukutake Sanchez
Read full bio of Swati Patwal
Read full bio of Rohit Garoo
Read full bio of Dr. Joyani Das