Image: Shutterstock
Strabismus refers to a condition in which one eye is directed to an object, while the other is misaligned (1). It is colloquially known as “crossed-eye,” “wandering eye,” or “squint.” Crossed eyes in infants are pretty standard and generally resolve after three to four months. However, in some cases, it might be a cause for concern. So how does one identify strabismus in babies, and what are its causes? In this post, we’ve compiled some information on the different types of strabismus, their symptoms, causes, and ways to treat the condition. Read on to know how you can help your baby.

Key Pointers
- Strabismus is a medical condition where one eye is not properly aligned with the object being looked at, causing the other eye to be misaligned.
- Strabismus in babies is caused by problematic eye muscles, damaged nerves, or neurological problems affecting muscle control centers in the brain.
- Symptoms of strabismus include eyes moving inward or outward, crossed eyes, one eye closed, and head turning to look at objects.
- Treatment options for strabismus include eye patching, corrective lenses, and surgery to adjust eye muscle length and position if necessary.
- Early medical attention is crucial for suspected strabismus as untreated cases can lead to lazy eye, impaired stereopsis, and developmental problems.
Signs And Symptoms Of Strabismus In Infants
It is normal for a newborn’s eyes to wander during the first few months of life since the little one is learning to focus. However, by the age of three to four months, the baby should be able to have a straight alignment of eyes and focus on objects.
Infants, who continue to have problems and develop strabismus, will display the following symptoms (2).
• Eyes moving inward
• Eyes moving outward
• Crossed eyes
• One eye closed
• Turning or tilting the head often to look at objects
Double vision is a common complaint with strabismus, but non-verbal babies cannot communicate it. Always seek a doctor’s opinion if you think that your baby has strabismus.
Is Strabismus Common In Infants?
Strabismus may occur at any age but is most common in infancy and childhood. According to the Harvard Medical School, strabismus affects up to 5% of children — both boys and girls equally (3).
What Causes Strabismus In Babies?
The basic cause of strabismus is a problem with the eye muscles. In rare cases, it can be a congenital disorder too. Strabismus might usually happen due to one or more of the following reasons (2) (4).
- Problematic eye muscles: There are six muscles attached to each eye to control eye movements. All the 12 muscles in both the eyes should work in sync to focus on one object at the same time. However, sometimes the muscles do not coordinate well, thus causing one eye to move in an abnormal direction, leading to eye muscle imbalance.
- Damaged or defective nerves: Three cranial nervesiA set of nerves that transport information from the brain to other body parts and support various sensory and motor activities are involved in supplying and controlling the eye muscles. An injury or defect in any of these nerves might lead to strabismus.
- Neurological problems: A problem with the control centers in the brain that direct the nerves and the eye muscles can also lead to strabismus.
Various factors might put an infant at a higher probability of developing strabismus and other vision development problems.
Risk factors for developing strabismus
- Heredity can cause strabismus. It is seen more commonly in babies whose direct family members have strabismus (2).
Shen-Li Lee, an author, speaker, and mother of two boys, expresses her concern about the likelihood of her children developing strabismus, “One of the reasons why I have been concerned about strabismus in Gareth (her son) is because hubby has “lazy eye” and so does my brother. With genes for eye problems running in both sides of the family, I suspect both Gavin and Gareth (her sons) may be susceptible to it (i).”
 Quick fact
Quick fact- Certain medical conditions such as hydrocephalusiAccumulation of excess cerebrospinal fluid in the brain ventricles (hollow cavities), causing severe pain and vision issues , cerebral palsyiA set of disorders affecting a person's ability to move, balance, and maintain proper postures down syndrome in babies (2) may increase the risk. Studies show that children with Down syndrome tend to develop strabismus at a significantly later age compared to children without the condition (5). Strabismus is significantly more common in children with cerebral palsy than in the general population. Research shows that around 49.8% of children with cerebral palsy in high-income countries and 39.8% in lower-income countries are affected by the condition (6).
- An injury to the eye or surrounding structures.
- Babies born preterm may be at a higher risk of developing strabismus (7).
- Prenatal exposure to drugs might cause strabismus in babies (8). For example, in several studies, maternal ingestion of a high dose of aspirin during pregnancy was found to increase the risk of strabismus
- Maternal smoking during pregnancy might also cause strabismus in babies (9). As per a study, smoking between five and 10 cigarettes a day increases the chances of the baby getting it by 38%. If a mother smokes 10 or more cigarettes per day, the risk nearly doubles compared to non-smokers (10).
- Individuals with uncorrected farsightedness (hyperopia) may develop strabismus due to the extra effort their eyes need to focus clearly on objects (11).
Diagnosis Of Strabismus
Most cases of strabismus are diagnosed before a child turns five years old, with about 90% of cases diagnosed within this age range. About 26% of the diagnosis occur within the first six months of life, as evident from the graph below.

Age distribution of strabismus diagnosis
Source: Incidence of strabismus, strabismus surgeries, and other vision conditions in Prader-Willi syndrome: data from the Global Prader-Willi Syndrome Registry; BMC OphthalmologyIf your baby is less than three months old, then the doctor may wait for the baby to cross four months before performing any eye exams or tests. If the signs of strabismus extend beyond three to four months of age, then the doctor may perform the following tests (12).
- Hirschberg test, which is a simple and quick test to determine incorrect eye alignment in babies (13). The test involves shining a small penlight on the infant’s eye. The doctor observes the reflection of the light in each pupil (the dark center of the eye). If the baby does not have strabismus, then the light’s reflection appears in the same position in each pupil. However, if the baby’s eyes are misaligned, then the position of the reflection will not be the same in each eye.
- The doctor will cover one eye of the baby, and the baby might be made to focus on an object like a colorful toy with the other eye. The same step is performed by covering the other eye. Strabismus can be confirmed if an uncovered eye does not remain straight but moves inward, outward, upward, or downward to focus on the object.
The doctor may request other tests if needed.
Consult a pediatric ophthalmology specialist to diagnose and plan further management for strabismus in your child.
Strabismus Treatment In Infants
Strabismus cases that go beyond three to four months of age may require treatment to prevent visual impairment.
- The unaffected eye is covered with an eye patch for several hours a day for weeks or months to force the brain to use the deviated eye. It helps stimulate adequate control of the eye muscles and restore normal vision (14).
- In some babies, strabismus might be corrected by wearing spectacles with the right type of lens required to correct the condition.
- Botox injections or botulinum toxiniA neurotoxic protein that affects the nervous system, produced by the bacterium Clostridium botulinum are used by doctors to temporarily paralyze specific eye muscles in children. This technique has been in use for over 30 years now. After the administration of these injections, you may see a momentary correction of your child’s squint initially, followed by a gradual realignment of the eyes as the temporary paralysis resolves. The effect of the medicine takes around two days to show its effect. This method tries to improve eye alignment, which may lead to fewer incidences of blurred or double vision. While the procedure is generally safe, following the suggestions of your child’s doctor is crucial (15) (16).
- If other methods do not improve the conditions, then surgical correction may be done. An eye surgery can be used to adjust the length and position of the affected muscles. It may also be required if strabismus is caused by damaged nerves (17).
Prognosis Of Strabismus
If you suspect your baby to have strabismus, it is good to seek medical attention as early as possible. Untreated strabismus can lead to the following conditions.
- Amblyopia: It is often called the “lazy eye.” It causes reduced vision in one or both eyes and reduced contrast sensitivity (18). According to a meta-analysis by researchers from The People’s Hospital of Leshan, the global prevalence of amblyopia in children is around 1.36% (19). Early detection and treatment of amblyopia can improve the prognosis of the condition (20).
- Impaired stereopsis: Stereopsis means the perception of depth that is created in the brain when both eyes look together at an object and produce a perfect image. Untreated strabismus can impair the perception of depth, thus causing vision problems, which might lead to other developmental problems in babies. A study found that children born with strabismus and absent stereopsis (depth perception) exhibited lower motor skills compared to those who developed strabismus later with normal stereopsis (21).
Rarely, persistent strabismus may be the first sign of childhood cataract, glaucoma, or tumors of the eye, optic nerve, or the brain (18).
Types Of Strabismus
Strabismus is classified according to the direction in which the eye turns under the following types (1).
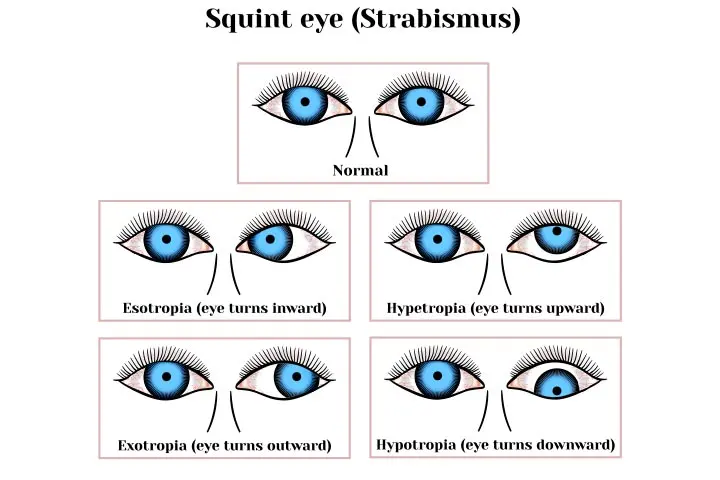
1. Inward turning is called esotropia
2. Outward turning is called exotropia
3. Upward turning is called hypertropia
4. Downward turning is called hypotropia.
Esotropia is the most common type of strabismus among children (9). There are a few variants of esotropia (22).
1. Infantile esotropia

It is usually associated with a family history of strabismus and can be diagnosed by the age of six months. Although mostly seen in healthy babies, it is prevalent in babies with hydrocephalus and cerebral palsy too.
 Quick fact
Quick fact2. Pseudostrabismus or pseudoesotropia

It is not true strabismus. The baby has a wide nasal bridge and extra fold of skin that gives an appearance of their eyes being crossed. The false appearance usually disappears as the baby grows, and the facial structure develops. A retrospective population-based cohort study found that approximately 1% of infants were born with pseudostrabismus over a 10-year period (23).
3. Accommodative esotropia

Often diagnosed at the age of two to three years, it is usually more common among children who have far-sightedness (medically known as hypermetropia) and thus cannot clearly see nearby objects. In such cases, the child’s eyes may misalign to focus on closer objects.
Strabismus is also classified according to other clinical features (2).
1. Continuous or intermittent, depending on the frequency
2. Unilateral, depending on the involvement of the same eye, every time
3. Alternating, when it happens in an alternate eye at a time
Frequently Asked Questions
1. Can my baby outgrow strabismus?
If strabismus persists after the age of four months, then the baby is unlikely to outgrow the condition without medical intervention (24). Treatment will be required to correct it.
2. Can strabismus cause developmental delays?
Studies have shown that strabismus may cause difficulty in achieving milestones like grasping, sitting, crawling, standing, and walking (25).
3. How long does it take to fix strabismus in babies?
It largely depends on the type of treatment and severity of the condition. In severe cases where surgical intervention is necessary, babies require around a few weeks to recover (1).
Infants may usually have cross eyes during the first few months of their life as they are still trying to learn how to focus their vision. However, this resolves three to four months after birth. If your baby is showing symptoms of ocular alignment disorders like strabismus even after the 4th month, see a pediatrician. Strabismus in infants may be treated using non-invasive and invasive manners. Since untreated strabismus could lead to lazy eye (amblyopia) in children, seeking prompt medical attention to address the condition is essential. Fortunately, strabismus has a good prognosis, provided it is identified and treated at the right time.
Infographic: Red Flags Associated With Strabismus
If strabismus in babies does not resolve after three months, they should be referred for further investigations as the condition may sometimes indicate other serious complications. This infographic will help you learn about those conditions and their red flags. Illustration: Momjunction Design Team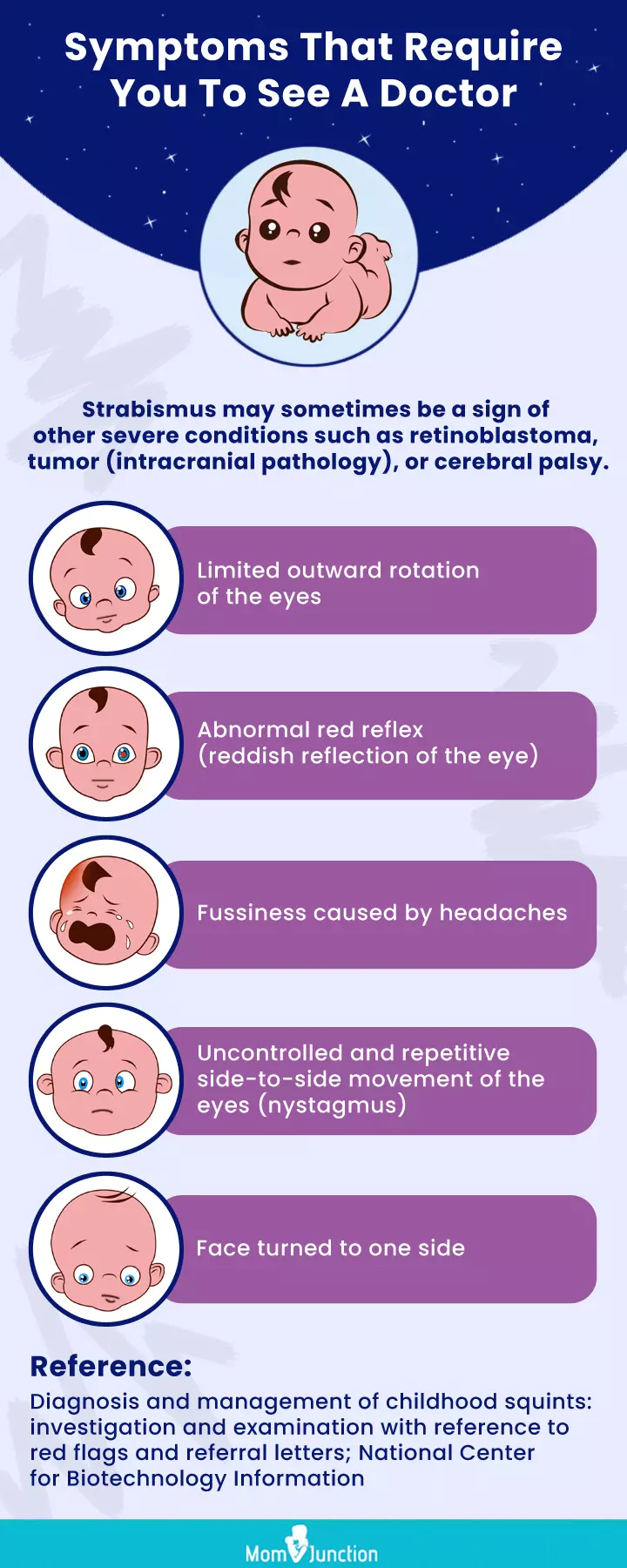
Illustration: Strabismus (Cross-Eye) In Infants: Signs Causes & Treatment
_in_infants_signs_causes__treatment_illustration.jpg.webp)
Image: Stable Diffusion/MomJunction Design Team
Learn all about Strabismus in this comprehensive video! Get the facts on what it is, causes, symptoms, and treatments. Get the answers you need to know!
Personal Experience: Source
MomJunction articles include first-hand experiences to provide you with better insights through real-life narratives. Here are the sources of personal accounts referenced in this article.
i. Babies: Strabismus, cross-eyes – When is it a problem?;https://nurtureforthefuture.wordpress.com/2010/01/29/babies-strabismus-cross-eyes-when-is-it-a-problem/
References
- Nicholas Sawers; Diagnosis and management of childhood squints: investigation and examination with reference to red flags and referral letters; The British Journal of General Practice
- Strabismus (Crossed Eyes). American Optometric Association
- Strabismus; Dean McGee Eye Institute
- Eugene M Helveston; Understanding, detecting, and managing strabismus; Journal of Community Eye Health
- Chand, Avishay, and Lingchen Wang., Prevalence and Etiology of Strabismus in Down Syndrome: A Systematic Review and Meta-analysis with a Focus on Ethnic Differences in the Esotropia/Exotropia Ratio; MedRxiv
- Herron, Michael S., and Lingchen Wang., Prevalence and Types of Strabismus in Cerebral Palsy: A Global and Historical Perspective Based on a Systematic Review and Meta-analysis; MedRxiv
- Deborah K. VanderVeen et al., Strabismus at Age 2 Years in Children Born Before 28 Weeks’ Gestation: Antecedents and Correlates; Journal of Child Neurology
- ELENA GHETAU, ROGER BLOOR & ALISON Y. FIRTH; Identification of strabismus in children born to mothers misusing substances during pregnancy: A clinical and research challenge; Researchgate
- Kerstin Strömland, M. Dolores Pinazo-Durán; OPHTHALMIC INVOLVEMENT IN THE FETAL ALCOHOL SYNDROME: CLINICAL AND ANIMAL MODEL STUDIES; Public Health and Epidemiology
- Boyd, Heather A., et al., In-Utero Exposure to Smoking, Alcohol, Coffee, and Tea and Risk of Strabismus; American Journal of Epidemiology
- Strabismus (crossed eyes); American Optometric Association
- Strabismus; Nemours KidsHealth
- ALIGNMENT ASSESSMENT (HIRSCHBERG); Moran Core Clinical Ophthalmology Resource for Education
- Strabismus in Children; American Academy of Ophthalmology
- Rowe FJ, Noonan CP, et al., Botulinum toxin for the treatment of strabismus; National Library of Medicine
- Botulinum toxin (Botox) injection for a squint; University Hospital Southampton NHS Foundation Trust
- Strabismus (Eye Misalignment); Cleveland Clinic
- Tailor V et al., Tests for detecting strabismus in children aged 1 to 6 years in the community; Cochrane Database Syst Rev. 2017
- Hu, Budan, et al., The Global Prevalence of Amblyopia in Children: A Systematic Review and Meta-Analysis; Frontiers in Pediatrics
- Rebekka Coles; Vision and eye health in children; the Pharmaceutical Journal
- Vagge, Aldo, et al., Motor Skills in Children Affected by Strabismus; Eye
- Esotropia; Cleveland Clinic
- Pseudostrabismus; American Academy of Ophthalmology
- What is Strabismus?; Optometrists Network
- Infantile Esotropia Linked to Developmental Delays; Elsevier
Community Experiences
Join the conversation and become a part of our nurturing community! Share your stories, experiences, and insights to connect with fellow parents.
Read full bio of Dr. Fadel Husrom
Read full bio of Dr. Ritika Shah
Read full bio of Rohit Garoo
Read full bio of Shinta Liz Sunny