Image: Shutterstock
Milk allergy in children occurs when a child’s immune system mistakenly perceives cow milk proteins as a threat and acts against them, triggering a reaction. A child allergic to milk develops symptoms when milk or milk-based foods are ingested. Depending on the severity of the allergic reaction, the symptoms may vary from mild to severe. Removing milk and milk products from the diet can help manage mild symptoms. In the US, milk allergy affects about 3% of children under three years (1). Fortunately, most children outgrow milk allergies before they turn 16. Thus, prompt treatment and management of the condition are essential for managing allergic reactions. Read this post to learn about the causes, symptoms, diagnosis, and treatment of milk allergy in children.

Key Pointers
- Milk allergy is an allergic reaction that occurs after your child consumes milk or milk products.
- There is no particular test for milk allergy in children, but your child’s medical, food, and family history may be useful.
- Avoid giving your children foods with ingredients such as whey protein, casein, lactose, protein hydrolysates, or milk solids.
- Your child’s nutritionist would devise a well-balanced milk-free diet plan with safe cow’s milk alternatives.
What Are The Causes Of Milk Allergy In Children?

There is no exact cause of milk allergy. Genetics and environmental factors may play a role in its manifestation. Physiologically, in those with milk allergy, the body identifies milk protein as an allergen and produces IgE antibodies. These antibodies bind to allergic cells (mast cells and basophils) in the body, and release chemicals called histamines that bring symptoms of an allergic reaction (2). Each time the child consumes milk or milk products, the body displays an allergic reaction (3).
 Quick fact
Quick factWhat Are The Symptoms Of Milk Allergy In Children?
Milk allergy symptoms may appear within two hours or several hours after the milk ingestion. If you suspect your child has a milk allergy, look for the following symptoms (1) (5).
- Red itchy rash or skin hives
- Swelling around the mouth, face, or around the eyes
- Runny or blocked nose; symptoms similar to hay fever
- Wheezing or shortness of breath and coughing
- Vomiting, abdominal cramps, or diarrhea, blood in stool
- Slow and poor weight gain
- In rare cases, cow milk allergy can cause anaphylaxis. Anaphylaxis is a life-threatening immune-response that impairs breathing and leads to a state of shock.
- If the gastrointestinal tract is affected, dehydration or failure to thrive can occur.
The intensity of symptoms varies from child-to-child. Also, milk allergy symptoms often seem similar to dairy sensitivity or lactose intolerance. Therefore, if your child shows intolerance symptoms, consult a pediatrician promptly for an accurate diagnosis.
 Point to consider
Point to considerHow Is Milk Allergy Diagnosed In Children?

There is no specific test that can detect cow milk allergy. Generally, the doctor will collect the family, medical, and diet history of your child along with a detailed discussion of the child’s symptoms. Based on these details, they are likely to advise the following tests (1) (5) (6).
- Elimination test: This simple test includes eliminating milk from the diet and then reintroducing it to see if it causes a reaction. If the pediatrician suspects milk allergy, they will recommend an allergist for further evaluation to confirm the diagnosis.
- Blood test: This test estimates the amount of total or specific immunoglobulin E (IgE) antibodies responsible for triggering an allergic reaction when a body is exposed to an allergen. However, this test does not help evaluate cow milk allergy with precision.
- Skin prick test: In this test, a liquid containing milk or milk protein extract is placed on the forearm or the back of the hand. The skin is then pricked with a small, sterile probe, allowing the liquid to enter the skin. The development of a raised, reddish bump, within 15 to 20 minutes indicates an allergy.
- Oral food challenge: In the test, your child will have to eat milk-based food in small but increasing quantities. If the child develops an allergy, it indicates a positive case of milk allergy. The test should only be performed in an allergist’s office with an emergency action plan ready due to its potential risk of causing a severe allergic reaction.
- Component test: This test can help an allergist determine the specific milk protein allergen for your child. It can help accurately determine the milk component that triggered the allergy.
Based on the diagnosis, your allergist will prescribe a treatment plan consisting of different treatment modalities.
What Is The Treatment For Milk Allergy In Children?

Milk allergy treatment aims at managing the triggers and symptoms. If your child is diagnosed with milk allergy, the treatment will include the following (5).
- Remove cow’s milk and its products from your child’s diet for a while. You are likely to be referred to a pediatric nutritionist who could devise a well-balanced milk-free diet plan with healthy cow’s milk substitutes.
- Use oral antihistamines to subside mild allergic symptoms, such as swelling, hives, a runny nose, and abdominal pain.
- Stay prepared with the use of an epinephrine auto-injector in case of a severe allergic reaction. Train your child on how to use the device. Encourage them to carry the injections with them at all times.
- Omalizumab (brand name Xolair®) is the first biologic medication approved for treating food allergies, including milk allergy. It is an anti-IgE injection that reduces the body’s allergic response and lowers the risk of severe reactions due to accidental milk exposure. Xolair is approved for children aged 1 year and older and is administered every 2 to 4 weeks (7).
Your child will undergo pediatric assessment every six to 12 months to know if they have outgrown the allergy.
What To Feed To Children With Milk Allergy?
A child on a dairy-free diet may be losing essential nutrients. However, you can offer a well-balanced dairy-free diet to mitigate the risk. Below are some foods that are nutritional alternatives of milk for toddlers and kids.
- Plant-based milk alternatives: A child may not be able to have milk due to milk allergy, but they can consume fortified soy milk, rice milk, oat milk, flax milk, almond milk, cashew milk, hemp milk, and coconut milk if they are not allergic to any of these foods (8) (9).
- Meat, poultry, and fish: Lean meat, poultry, and fish are excellent sources of high-quality protein and micronutrients, such as calcium, vitamin A, vitamin D, vitamin B12, iron, zinc, and potassium (10). You can offer these foods to your child as a part of a well-balanced diet.
- Calcium-rich veggies and fruits: Kale, amaranth, broccoli, okra, and spinach are some calcium-rich veggies that can add color, flavor, texture, and valuable nutrients to your child’s diet (11). Similarly, rhubarb, blackberries, and kiwi fruit can be healthy alternative sources of calcium that work as a substitute for dairy products (12).

- Pulses, legumes, and nuts: These foods offer protein, healthy fats, and essential micronutrients, such as iron and zinc (10). You can feed them to your child as a part of a well-balanced diet.
- Fortified foods: Fortified foods, such as fortified cereals and health drinks, can be added to a child’s diet. You can speak to a pediatrician who can recommend a fortified cereal or health drink based on your child’s age.
- Milk-free breads: Breads and grain products made without milk or milk derivatives are also a safe as well nutritious option. Eating whole grains helps kids grow and develop, and offering them early encourages healthy eating habits that last a lifetime (13).
Eating a well-balanced diet ensures that a child gets all the necessary nutrients in optimum amounts. Consider consulting a dietitian to ensure your child receives a balanced diet and a personalized meal plan to prevent deficiencies while managing their allergy.
What Are The Complications Of Milk Allergy In Children?
While many outgrow it, the condition can lead to several short- and long-term complications if not properly managed. Children with milk allergy may have a higher risk of experiencing the following complications.
- Insufficient supply of vital nutrients that can hinder the growth and development of a child. In such cases, along with a well-balanced diet, nutritional supplementation may be necessary for some time to ensure the child’s uninterrupted growth and development (5).
- Allergies in children may occur due to other foods, such as peanuts, eggs, and soy. Research shows that children with milk allergy are more likely to develop other food allergies (5). For instance, 50% of infants with cow milk allergy may also have a cross-reaction with soy protein, notes the American Academy of Pediatrics (AAP) (9).
- Allergic colitis: This inflammatory condition affects babies and pre-school children. It can be caused by an immune reaction to cow’s milk proteins. Common signs include bloody stools and abdominal pain (14).
Zoe, a mother of a child with cow’s milk protein allergy (CMPA), recounts how she discovered her daughter, Alyssia, might also be allergic to soy products, “At around 3 months old – Alyssia was diagnosed with CMPA and was put onto aptamil pepti 1 milk. The doctors told us that she might grow out of it, and that this could just be a temporary thing but we have noticed that she gets the same reaction with soya products & after the last time (swelling eyes, diarrhoea, eczema rash, colic & vomiting) I am very nervous to try her on any of those foods again (i).”
Poor nutrition, due to the absence of milk in the diet, can be mitigated through alternative food items. Parents of children with milk allergy should be alert to the presence of other allergies.
How To Prevent Milk Allergy In Children?

You cannot prevent milk allergy, but allergic reactions attributed to milk allergy can be prevented by avoiding milk and milk products. Below are some steps that you should educate your child to manage milk allergy effectively (15) (16) (17).
- Avoid all kinds of milk, such as whole, skim, low-fat, evaporated, condensed, and powdered milk.
- Eliminate milk products, such as clarified butter, butter, butterfat, butter oil, cream, cheese, cottage cheese, yogurt, etc, from the diet.
- Avoid foods prepared from milk and its products, such as hot cocoa, candies, chocolates, eggnog, milkshakes, French toast, custard, ice cream, salad dressing, and pudding.
- Check food labels carefully while buying packaged foods. The “non-dairy” label on a product means it does not contain butter, cream, or milk. But the product may have other hidden sources of milk.
- A “lactose-free” label does not mean the product is dairy-free. Such products may still contain some milk proteins. Baked goods, such as cookies, and cereal products, such as bread and pancakes, are examples of such products.
 Quick tip
Quick tip- Some processed foods or pre-cooked products may also contain milk as artificial butter flavors, such as margarine and non-dairy creamers. Luncheon meat, hot dogs, and sausages contain milk as a meat binder.
- Avoid products containing whey protein, casein, protein hydrolysates, lactose, or milk solids in their ingredient list.
- Children allergic to cow milk may be allergic to sheep milk, goat milk, and the milk of other animals (19). In such cases, the doctor may ask your child to avoid animal milk entirely.
- Some medicines, such as antibiotics, probiotics, and even vaccines, may contain casein, a milk protein. Inform your doctor about your child’s milk allergy before they write a prescription (20).
- Whenever you visit a restaurant, inform the chef that you have a milk allergic visitor with you so that they avoid milk products in the food.
- Sometimes, breastfed babies might also develop symptoms of milk allergy. In such cases, the doctor might advise you to eliminate cow’s milk from your diet. Hydrolyzed formulas may be recommended for formula-fed babies (21). Amino acid formula is another option, but it is usually avoided due to its high cost and bad taste (22).
- If you use Kosher foods, avoid using foods labeled with a “D” or “DE” adjacent to Kosher symbols. It indicates that the product may contain traces of milk or is manufactured on machinery that handles milk or milk products.
- Provide detailed information about your child’s milk allergy to caregivers, teachers, and school nurses. This includes a list of safe and unsafe foods, symptoms of allergic reactions, and emergency contact information.
- Always double-check food labels, even on products you’ve bought before, since ingredients can change without warning.
- Prevent cross-contamination by cleaning all cooking tools, surfaces, and appliances carefully to avoid contact with milk, as even small traces can trigger a reaction (23).
- Make sure that everyone responsible for your child’s care, such as teachers, school nurses, and babysitters, knows about the allergy. Share clear information with them, including safe and unsafe foods, signs of an allergic reaction, and emergency contact details.
Frequently Asked Questions
1. Can a child suddenly become allergic to milk?
While milk allergy is most common in young children, it may develop at any point of time in life. You may develop an allergic reaction even by eating milk-containing products that your child may have tolerated well in the past (24).
2. What are kids allergic to in milk?
Milk proteins such as casein, alpha-lactalbumin, and beta-lactalbumin may be responsible for milk allergies in children (1) (25). Some children don’t produce sufficient lactase enzymes to break the lactose. Hence, they find it difficult to digest it and are allergic to milk.
3. Do milk allergies get worse with age?
According to studies, with the maturation of the digestive system, over 90% of children outgrow the allergy by the time they are six years old (5).
Milk allergy in children can cause concern in the parents and the child. Genetic and environmental factors can trigger this allergy in your child. The condition can manifest as a red itchy rash; runny nose; swelling around the mouth, face or eyes; or abdominal cramps. Milk allergy in children can be treated by removing cow’s milk from their diet and using oral antihistamines. However, ensure you are mindful of the symptoms, and if your child has an allergy, offer them a wholesome milk-free diet.
Infographic: Is Oral Immunotherapy Effective In Cow’s Milk Allergy?
It is difficult to completely avoid milk and dairy products as they are a part of several processed foods. Although a long-duration treatment, children with cow’s milk allergy may benefit from oral immunotherapy (OIT). The infographic below highlights the salient points of the therapy.
Some thing wrong with infographic shortcode. please verify shortcode syntax
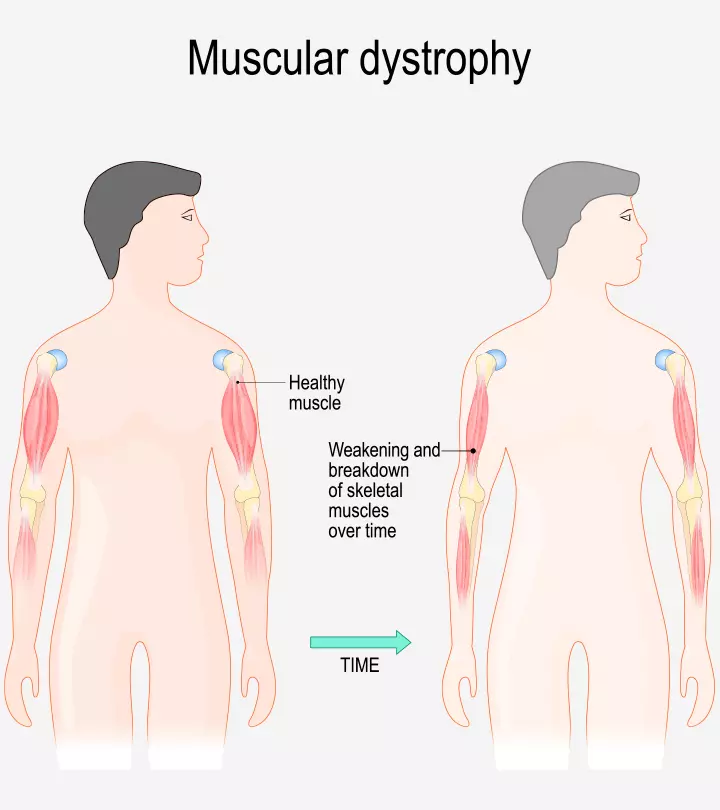
Illustration: Important Signs And Causes Of Milk Allergy In Children

Image: Stable Diffusion/MomJunction Design Team
Learn how to cure milk allergy and how to identify and manage its symptoms. Explore efficient treatments and lifestyle changes that can improve your overall health.
Personal Experience: Source
MomJunction articles include first-hand experiences to provide you with better insights through real-life narratives. Here are the sources of personal accounts referenced in this article.
i. My Experience of a Cows Milk Protein Allergy (CMPA) Baby;https://mummyandliss.wordpress.com/2017/01/25/my-experience-of-a-cows-milk-protein-allergy-cmpa-baby/
References
- Milk & Dairy.
https://acaai.org/allergies/allergic-conditions/food/milk-dairy/ - Milk Allergy.
https://www.foodallergy.org/living-food-allergy/food-allergy-essentials/common-allergens/milk - Histamine: The Stuff Allergies are Made of.
https://medlineplus.gov/medlineplus-videos/histamine-the-stuff-allergies-are-made-of/ - Cow’s Milk Protein Intolerance.
https://www.urmc.rochester.edu/childrens-hospital/gastroenterology/conditions/cow-s-milk-protein-intolerance - Cow Milk Allergy.
https://www.ncbi.nlm.nih.gov/books/NBK542243/ - Milk Allergies.
https://www.chop.edu/conditions-diseases/milk-allergies - Milk Allergy: Causes Symptoms Diagnosis & Treatment.
https://allergyasthmanetwork.org/food-allergies/milk-allergy/ - Milk Alternatives.
https://www.kidney.org/kidney-topics/milk-alternatives - Cow’s Milk Alternatives: Parent FAQs.
https://www.healthychildren.org/English/healthy-living/nutrition/Pages/milk-allergy-foods-and-ingredients-to-avoid.aspx - Meat Poultry Fish Dry Beans Eggs and Nuts.
https://www.umass.edu/nibble/infofile/meats.html - Get calcium and vitamin D by growing and eating vegetables and fruit.
https://www.canr.msu.edu/news/get_calcium_and_vitamin_d_by_growing_and_eating_vegetables_and_fruit - Calcium Content of Foods.
https://www.ucsfhealth.org/education/calcium-content-of-foods - New Age-Specific Dietary Guidelines Emphasize Whole Grains for Kids.
https://wholegrainscouncil.org/blog/2025/01/new-age-specific-dietary-guidelines-emphasize-whole-grains-kids - Ulcerative colitis in children.
https://www.cicra.org/what-is-ibd/ulcerative-colitis/ - Cow’s Milk Free Diet Information for Babies and Children.
https://www.allergyuk.org/resources/cows-milk-free-diet-information-for-babies-and-children/ - Milk Allergy Diet.
https://www.chop.edu/conditions-diseases/milk-allergy-diet-children - Milk Allergy Diet for Children.
https://www.stanfordchildrens.org/en/topic/default?id=milk-allergy-diet-for-children-90-P01696 - Food allergies.
https://www.schn.health.nsw.gov.au/kids-health-hub/kids-nutrition/food-allergies-children - Cow’s milk allergy.
https://www.betterhealth.vic.gov.au/health/ConditionsAndTreatments/cows-milk-allergy - John M. Kelso; (2014); Potential food allergens in medications.
https://www.jacionline.org/article/S0091-6749(14)00432-1/pdf - Herbert Brill; (2008); Appoach to milk protein allergy in infants.
https://www.cfp.ca/content/54/9/1258.short - Carlo Caffarelli et al; (2010); Cow’s milk protein allergy in children: a practical guide.
https://pmc.ncbi.nlm.nih.gov/articles/PMC2823764/ - Milk Allergy.
https://kidswithfoodallergies.org/living-with-food-allergies/top-food-allergens/milk-allergy/ - Milk Allergy.
https://my.clevelandclinic.org/health/diseases/11315-milk-allergy - How to spot a cow’s milk protein allergy.
https://childrenswi.org/at-every-turn/stories/milk-protein-allergy
Community Experiences
Join the conversation and become a part of our nurturing community! Share your stories, experiences, and insights to connect with fellow parents.
Read full bio of Dr. Anuradha Bansal
Read full bio of Swati Patwal
Read full bio of Rohit Garoo
Read full bio of Shinta Liz Sunny