Image: ShutterStock
Obstetric cholestasis (OC) or intrahepatic cholestasis of pregnancy (ICP) is a rare liver condition that affects 0.5% to 2% of pregnant women(1)

. The condition is more commonly seen in Araucanian Indians and females of Scandinavian ancestry (2).
Women dealing with ICP have reduced bile flow in the intestine, which eventually accumulates bile salts in the blood, causing itchy skin and other symptoms. ICP can occur due to several reasons, but the symptoms disappear after delivery in most cases.
This post informs you about ICP, including its causes, symptoms, diagnosis, treatment options, and recommended dietary changes to manage it.
Key Pointers
- Obstetric cholestasis reduces bile flow into the intestines, causing bile salts to build up and leak into the bloodstream.
- The cause of obstetric cholestasis is unknown, but it is influenced by hormones, genetics, and the environment.
- The main symptom of the condition is severe itching in the last trimester of pregnancy, and it is often diagnosed through blood tests.
- Relief from itching can be found through cool baths, creams, mild soap, loose clothing, and avoiding heat and alcohol.
- Treatment involves doctor-prescribed medications and a balanced diet including fruits, vegetables, low-fat, and high protein foods.
What Is Obstetric Cholestasis?
Obstetric cholestasis is a condition that reduces the normal outflow of bile from the liver.
Normally, the liver produces bile, which flows through the bile ducts into the intestine, where it helps in digesting the food.
But in the case of obstetric cholestasis, the bile flow into the intestines is reduced. This builds up the bile salts, which leaks into the bloodstream and increases the amount of bile salts in the blood.
The excess salts make your skin very itchy, causing a condition called pruritus. This usually occurs in the last three months of pregnancy, and sometimes even sooner. But the good thing is that raised bile salts and pruritus disappear after delivery, and do not cause any long-term complications for the mother or the baby (3).
What Causes Obstetric Cholestasis?
The exact cause of cholestasis during pregnancy is not known. However, it is known to be affected by the following factors (4):
- Hormonal: An increase in the pregnancy hormones, estrogen and progesterone, can affect liver function. Studies show that obstetric cholestasis usually occurs in the last trimester when the estrogen levels are higher. It is also common in twin and triplet pregnancies when the hormonal levels are high.
- Genetic: In some cases, obstetric cholestasis may runs in families (but can skip some generations). Those with a genetic predisposition to OC can also inherit a problem associated with bile production and passage through the bile ducts. OC may not be a major concern unless you are pregnant, as an increase in hormonal activity during pregnancy can result in hormonal changes.

- Environmental factors: OC is more common during winters, and the incidence is high when combined with nutritional factors like selenium deficiency (4).
Whatever might be the cause, this condition occurs only during pregnancy.
What Are The Symptoms and Signs Of Intrahepatic Cholestasis Of Pregnancy/ Obstetric Cholestasis?

The most common symptom of obstetric cholestasis is itching, which usually develops without a rash. It may start after 24 weeks of pregnancy when the hormone levels are at their peak. However, most women may have severe itching during the last trimester of pregnancy. The following characteristics of itching can be seen during cholestasis of pregnancy.
- It occurs on the palms and soles, but it can also affect other areas of the body.
- The itching gets worse at night and tends to worsen, until you have your baby.
- The itch can be mild to severe.
- Severe itching can affect your sleep pattern, your mood, and concentration.
Other symptoms, although rare, include (5) :
- Tiredness
- Feeling sick or ill
- Dark urine color
- Pale stools
- Food aversions
- Mild jaundice, characterized by yellow urine, skin, or whites of the eye
- Pain around the liver, usually in the right upper quadrant
- Nausea
- Depression
- Fatigue
Occasional, mild itching is normal. But if you develop a constant itch that turns worse in combination with the above symptoms, you should see your doctor immediately.
A mother of two recalls the symptoms that led to her getting diagnosed with cholestasis during her second pregnancy. She says, “I suddenly began experiencing severe itching around 36 weeks. Now, when I say that my palms & soles were itchy, I don’t mean that I randomly scratched every now and then. The itching intensified at night, and I would be awake and scratching at myself for hours every night. I’d use a rough washcloth and rub it against my hands & feet for hours on end. A few times, I scratched myself with my wig brush because the stiff bristles felt good, even if they made my skin red and sore. Nothing gave me any relief other than eventually passing out from exhaustion, and even then, I’d wake up scratching.
“(When she visited a doctor), the doctor mentioned that itchy hands and feet could be a symptom of cholestasis of pregnancy (CP or ICP), and he wanted me to go to the lab right away to get blood drawn. My liver function, as indicated by enzyme levels, and my bile acid levels were what he specifically wanted to see. I went to the lab late that day, and the results indicated that a specific enzyme was four times over the upper normal level (i).”
How Is Obstetric Cholestasis Diagnosed?
Obstetric cholestasis is diagnosed through blood tests. Your doctor will discuss your symptoms, your family history, and medical history, and recommend some tests to measure the bile acids and liver enzymes.
These tests will check for obstetric cholestasis and also detect other causes of itching.
- Bile acid test: This is the most specific test for OC. It measures the levels of bile acids in the bloodstream. The normal range is 0-10 micromol/L, and any reading above this range detects the presence of OC (6).
- Liver function test (LFT): It checks the functioning of the liver by measuring the different enzyme levels. The primary enzymes including, alanine transaminase (ALT) and aspartate transaminase (AST), will rise abnormally in the case of OC.
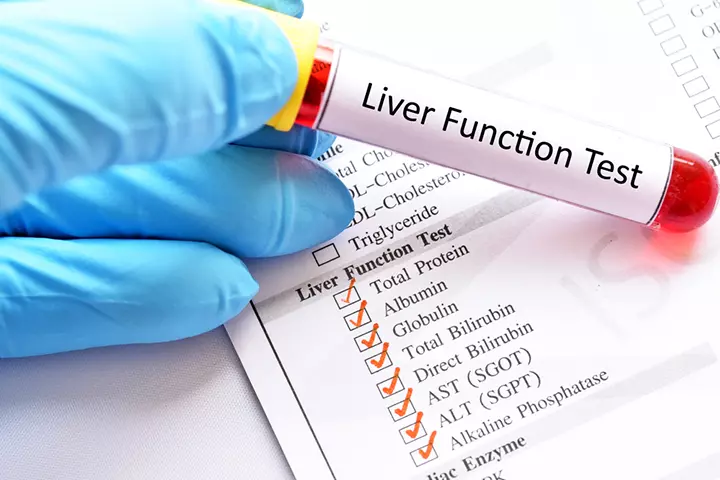
Sometimes bile acid levels rise while the ALT and AST remain normal. In other cases, there may be elevated liver enzymes while the levels of bile acids remain normal. In both cases, your bile acids are tested if there is recurrent itching (7).
What Are The Risks Of Obstetric Cholestasis?
For the mother-to-be, obstetric cholestasis can lead to vitamin K deficiency and affect the body’s ability to clot blood. There is an increased risk of bleeding as it takes a longer time to stop. However, the research behind this is indefinite. Your doctor will suggest vitamin K supplements to treat the clotting problem (8).
You may undergo more antenatal appointments so that the doctor can examine you carefully. The medical tests involve:
- Tracking the baby’s movements
- Listening to the baby’s heartbeat
- Fetal monitoring using ultrasound scans to track the growth and well-being of the baby.
For the unborn baby
- Your baby may pass their first stool (meconium) while still in the womb. It could, therefore, cause breathing problems post birth.
- You may go into preterm labor if your doctor advises an early delivery.
- There is an increased risk of stillbirth, which is why the doctor suggests induced labor at around 37 to 38 weeks (9).
 Quick fact
Quick factIf you have a high-risk pregnancy and suffer from obstetric cholestasis that is too severe, your obstetrician may decide to induce labor before 37 weeks, based on your blood tests and bile acid levels in the blood (10).
How Is Obstetric Cholestasis Treated?
The primary goal of the treatment is to relieve itching. The following measures may help to alleviate itching associated with obstetric cholestasis (11):
- Cold water baths
- Soaking feet and hands in ice water
- Applying calamine lotion on itchy regions

 Quick tip
Quick tipThe above measures can offer temporary relief, especially before bedtime, so that the itch may ease and allow you to have a good night’s sleep.
Medical Treatment For Managing Cholestasis During Pregnancy
Medication is usually aimed at decreasing the bile salt levels, relieving itching, and protecting the baby. Your doctor is likely to prescribe the following medications for obstetric cholestasis.
- Ursodeoxycholic acid (ursodiol), which eliminates the itching, and normalizes the liver and bile acids (11).
Nevertheless, using ursodeoxycholic acid in the treatment does not decrease unfavorable outcomes for newborns. A UK-based research study primarily assessed a comprehensive measure incorporating perinatal mortality, premature birth, or admission to a neonatal unit. Out of the 322 babies who received ursodeoxycholic acid, about 23% had one of these negative outcomes. On the other hand, in the group of 318 babies who received a placebo, about 27% had one of these negative outcomes. This suggests that using ursodeoxycholic acid did not significantly reduce the probability of negative outcomes.
- Steroids (dexamethasone) with careful management. They aid in the maturity of the baby’s lungs (12).
- Vitamin K supplements to help with blood-clotting (6).
Note:
Do not use antihistamines, aveeno, and oatmeal baths.
Diet For Intrahepatic Cholestasis
The primary goal of the pregnancy cholestasis diet is to place less strain on the liver, and for that, you should be taking foods containing lecithin, which is unsaturated fat that helps absorb fats in the bile. A low-fat diet may make it easy for the intestine to absorb vitamins and minerals from the food. Include:
- A mix of organic fruits and vegetables with colorful pigments such as carrots, beets, potatoes, pumpkin, red cabbage, and cauliflower for easy digestion.
- Foods containing omega-3 fatty acids (tuna, salmon, mackerel, sardines, shrimp, oysters, linseed, and cod liver oils) and omega-6 fatty acids (leafy greens, nuts, fish, and soybeans) to combat illnesses.
- High protein foods, including nuts, beans, fish, and eggs.
- A low-fat diet of rice, wheat, corn, oats, and rye.
- Virgin olive oil, sunflower oil, and canola oil.
- Healthy alternatives such as honey spread, hummus, and fruit jams.
- More water to flush away toxins from the system.
- Fresh lemon juice in warm water to neutralize the bile acids.
This diet helps minimize bile production in the liver and promotes liver health. Besides a healthy diet, other natural remedies can be used to deal with obstetric cholestasis.
Natural Remedies For Obstetric Cholestasis
Before going for medical treatment options, you can try the following measures to lower the discomfort associated with obstetric cholestasis. These remedies also reduce the chances of developing the condition. Do check with your doctor about them.
- Guar gum: Guar gum is a fiber component of the seed of the guar plant. Research shows that oral intake of guar gum relieves cholestasis. It binds to the bile, thereby preventing an increase in serum bile levels (13). You should ask your doctor about it.
- Activated charcoal: This is a potent treatment method where activated charcoal traps chemicals and toxins in the body, allowing them to flush out before they get absorbed. In a study, it was found that an eight-day treatment of activated charcoal reduced bile concentrations in pregnant women with ICP (14). Ask your doctor first.
- Dandelion root: It is a safe remedy for gallstones, one of the significant causes of cholestasis. The vitamins and nutrients in dandelions aid in cleansing the liver and stimulating proper bile flow (15).

- Vitamin D and calcium: Research findings show that metabolic bone diseases are a complication of cholestatic liver disease (16). Therefore, it is also essential that you consume calcium-rich foods and calcium supplements. Vitamin D, which you can get by spending some time outdoors, also plays a key role in absorbing calcium (17).
Along with these natural remedies, maintaining a consistent exercise or meditation routine can help reduce stress levels, which may worsen itching when elevated.
While taking these measures helps manage the condition better, medical supervision is necessary for a few weeks to months, even after delivery.
Obstetric Cholestasis Or Intrahepatic Cholestasis Of Pregnancy After Delivery
A follow-up check-up is done around six to eight weeks after the baby is born. Your doctor will check if the itch is still there and if the liver is working normally.
- If you are using birth control pills, you may be told to stop them as the estrogen in them can trigger cholestasis again. The doctor may suggest an alternative contraceptive.
- You may be at risk of developing chronic liver disease and gallstones in later life.
- There is a 45-70% chance that obstetric cholestasis recurs during subsequent pregnancies (4).
Frequently Asked Questions
1. What foods should I avoid if I have cholestasis in pregnancy?
You should avoid the following foods if you have cholestasis during pregnancy (18).
- Foods with a high amount of sugar or artificial sweeteners
- White flour and soy products
- Processed meats
- Eat dairy products in small portions and avoid full-fat milk, cream, and cheese
- Foods with high caffeine content
2. Can cholestasis of pregnancy be prevented?
No, cholestasis of pregnancy cannot be prevented. However, timely and accurate diagnosis and treatment are essential to minimize the risk of adverse effects on maternal and fetal health (19).
3. Can intrahepatic cholestasis of pregnancy affect future pregnancies?
Intrahepatic cholestasis of pregnancy may recur in future pregnancies and babies. However, babies born to mothers that suffer from this disease have normal development but may be at sufficient risk of contracting metabolic diseases (21).
There are several hormonal, environmental, and genetic factors that could cause intrahepatic cholestasis of pregnancy which may cause irresistible itching. This condition may also impact your eating patterns by causing food aversions, nausea, and abdominal discomfort. If you notice any of the symptoms of intrahepatic cholestasis like pale stools, jaundice, or dark-colored urine, consult your doctor for prompt medical intervention. The treatment usually aims at reducing the intensity of the itches through medications and vitamin K supplementations. In addition, you may have to follow a low-fat diet.
Infographic: Which Conditions May Mimic Intrahepatic Cholestasis Of Pregnancy?
Symptoms such as pruritus and jaundice can be seen in various health conditions in pregnancy, requiring prompt medical care. Mistaking them for intrahepatic cholestasis of pregnancy can delay the adequate treatment on time. Check out the infographic to know common health conditions that mimic intrahepatic cholestasis of pregnancy. Illustration: Momjunction Design Team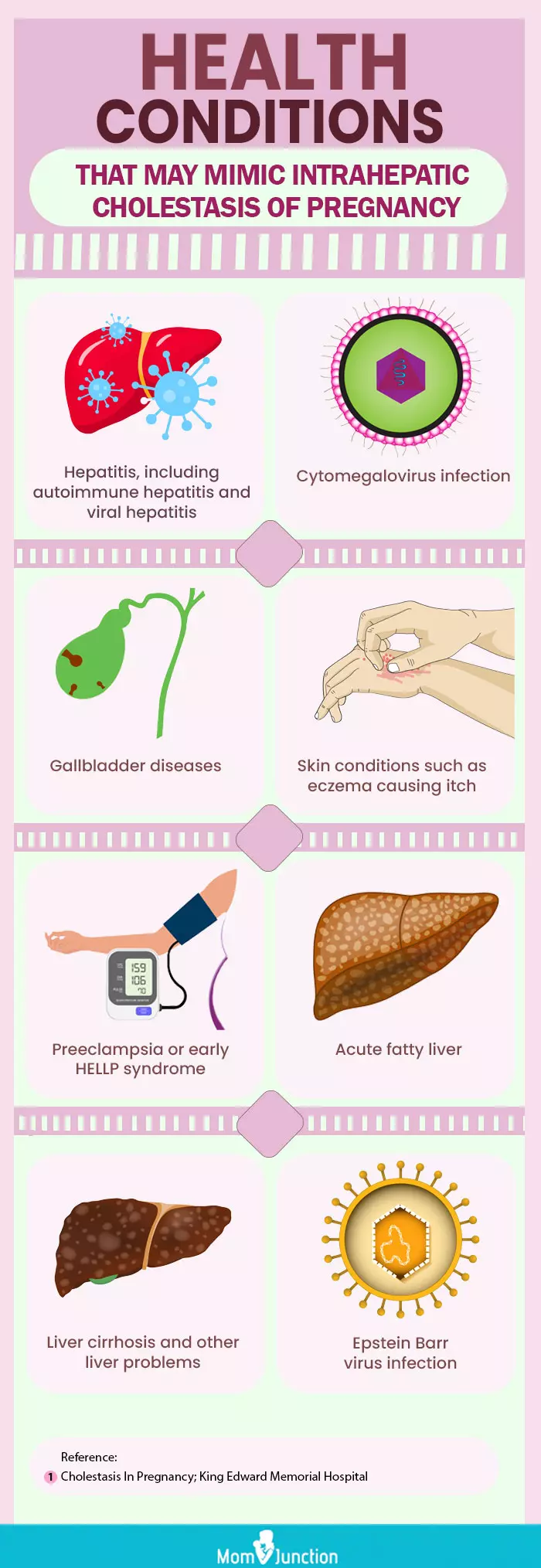
Learn more about Cholestasis in Pregnancy to better understand its symptoms, treatment techniques, and diagnostic processes. Discover insights and beneficial strategies for successfully managing this condition.
Illustration: Intrahepatic Cholestasis Of Pregnancy: Symptoms & Causes
Image: Stable Diffusion/MomJunction Design Team
Personal Experience: Source
MomJunction articles include first-hand experiences to provide you with better insights through real-life narratives. Here are the sources of personal accounts referenced in this article.
i. Cholestasis of Pregnancy;https://bloggymcbloggerstein.blogspot.com/2012/02/cholestasis-of-pregnancy.html
References
1. Maternal cholestasis during pregnancy programs metabolic disease in offspring; J Clin Invest.
2. Intrahepatic cholestasis of pregnancy; The National Institutes of Health (NIH)
3. Tan LK; Obstetric cholestasis: current opinions and management.
4. Thomas Pusl and Ulrich Beuers; Intrahepatic cholestasis of pregnancy
5. Cholestasis Of Pregnancy; The American Pregnancy Association
6. Maria Maldonado, et al.; Intrahepatic Cholestasis of Pregnancy Leading to Severe Vitamin K Deficiency and Coagulopathy
7. Yannick Bacq.; The Liver in Normal Pregnancy
8. Obstetric cholestasis in Hong Konglocal experience with eight consecutive cases; Department of Obstetrics and Gynaecology, Kwong Wah Hospital, Kowloon, Hong Kong
9. Cholestasis of Pregnancy; The University of Rochester Medical Center
10. Maria C. Estiú, et al.; Relationship between early onset severe intrahepatic cholestasis of pregnancy and higher risk of meconium-stained fluid
11. Obstetric cholestasis in Hong Kong—local experience with eight consecutive cases; HKMJ
12. Elizabeth Gialanze, et al.; Use of dexamethasone in the management of intrahepatic cholestasis of pregnancy – case report
13. Gylling H, et al.; Oral guar gum treatment of intrahepatic cholestasis and pruritus in pregnant women: effects on serum cholestanol and other non-cholesterol sterols.
14. Kaaja RJ, et al.; Treatment of cholestasis of pregnancy with peroral activated charcoal. A preliminary study.
15. Dandelion; The National Center for Complementary and Integrative Health
16. Isaia G, et al.; Bone disorders in cholestatic liver diseases.
17. Bengoa JM, et al.; Intestinal calcium absorption and vitamin D status in chronic cholestatic liver disease.
18. Diet for Intrahepatic Cholestasis of Pregnancy (ICP); ICP Care
19. Cholestasis of pregnancy; Cleveland clinic
20. Itching and intrahepatic cholestasis of pregnancy; NHS, UK
21. Rebecca Roediger and Jaquelyn Fleckenstein; (2025);Intrahepatic Cholestasis of Pregnancy: Natural History and Current Management; NCBI
Community Experiences
Join the conversation and become a part of our nurturing community! Share your stories, experiences, and insights to connect with fellow parents.
Read full bio of Dr. Mozhgan Sayyad
Read full bio of Rebecca Malachi
Read full bio of Swati Patwal
Read full bio of Aneesha Amonz

















