Image: ShutterStock

Uterine abnormalities during pregnancy might cause complications if not treated at the earliest. The uterus is the most important part of the reproductive system as it provides nourishment and protection to the developing fetus. Thus, it is important to consult with your doctor before trying for a baby. The common symptoms of uterine abnormalities are pain during menstruation or sex, followed by bleeding, recurrent miscarriages, or difficulty in getting pregnant. Although a minor surgery could help, it is better to consult the doctor during the initial days to continue a healthy, full-term pregnancy. Read on to know about uterine abnormalities, their causes, symptoms, and treatment options.
Facts About Uterine Abnormalities
As strange as it may sound, uterine abnormalities are not rare. Hence, it is crucial you understand a few things about these anomalies.
Uterine abnormalities don’t exhibit many signs or symptoms.
Some uterine anomalies are diagnosed in puberty. Many uterine abnormalities may not even cause any pain or complications with your pregnancy.
Certain uterine abnormalities may result in miscarriages or preterm births. A doctor can analyze these abnormalities only when you are trying to conceive actively, or you fall pregnant (1).
Some uterine abnormalities present conditions that need medical intervention to improve your chances of having a healthy, uncomplicated pregnancy.
What Are Congenital Uterine Abnormalities?
Congenital uterine abnormalities are rare, but they do occur. Less than 5% of women have congenital uterine anomalies (1). A congenital condition is typically present at birth. So, if you have a congenital abnormality of the uterus, it means you were born with the defect. Usually, your uterus develops while you are growing in the womb as two sections. These two parts fuse before birth.
Fascinating congenital abnormalities of the uterus are müllerian duct anomalies. Between the 6th and 11th week of pregnancy, the müllerian ducts fuse to form the fallopian tubes, uterus, proximal two-thirds of the vagina, cervix in a female fetus (2).
Sometimes this fusion doesn’t occur properly, leading to defects in the internal reproductive organs. Usually, these abnormalities are linked to the working of the ovaries or the external genitalia. In most cases, the anomalies become apparent with the onset of puberty. Before puberty, the abnormalities of the internal reproductive organs are not visible or noticeable. Usually, gynecologists diagnose the problem after a young woman approaches them for menstrual disorders.
Can Congenital Uterine Anomalies Affect Pregnancy?
Whether uterine defects will cause pregnancy-related issues or not depends primarily on the type of abnormality. In most cases, women with uterine anomalies can conceive naturally, and they won’t even realize that they have a defective uterus. These abnormalities may, however, determine whether the pregnancy will continue full term or the woman will have a miscarriage.
Remember uterus is another name for your womb. So it goes without asking that any defect of the uterus will have a profound effect on your pregnancy. Nevertheless, there are also a few uterine conditions that may not have a significant impact, and if you have one of these conditions, you may still be able to deliver a healthy baby with or without medical intervention. This said it is more common for a pregnancy to develop problems in case of uterine anomalies, or the following issues may further aggravate due to the defects (3):
1. Premature Birth:
Most uterine conditions can result in premature birth. Premature birth is when the delivery happens too early, before 37 weeks of pregnancy. Preterm births pose health risks to the newborn as his immunity is not entirely developed to survive outside the womb. Also, in some babies, lung development may not be complete. If you have a preterm baby due to a uterus-related defect, he will require specialized neonatal care until the neonatologist deems it necessary (4).
2. Slow Fetal Growth:
Uterine anomalies may cause your baby to develop slowly inside the womb as well as post-birth. Some of the most common developmental issues with infants occur when a woman has a uterine defect. Due to an abnormal uterus, your baby may not get the nourishment required for optimal growth.
3. Breech Position:
Uterine anomalies may result in the baby entering the breech position (fetal malpresentation) inside the womb. In this position, your baby’s bottom or feet are facing down instead of the head. Such pregnancies do not significantly impact the fetus’ viability but may require a planned Cesarean delivery. Also, sometimes, such pregnancies may not reach the full term (5).
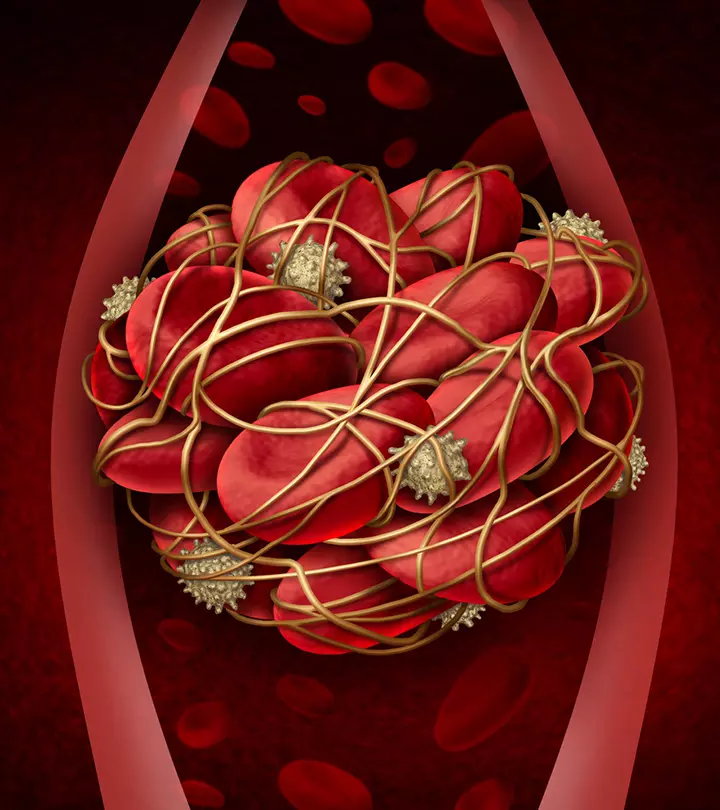
4. Miscarriage:
Miscarriages are the most common result of uterine anomalies. Most women with abnormalities of the uterus will encounter one or more miscarriages. It is often after a miscarriage that some of these uterine anomalies become significantly evident as they may not present any symptoms prior to the pregnancy and subsequent miscarriage.
Causes Of Müllerian Duct Anomalies
Müllerian duct anomalies are congenital abnormalities. Hence, if you have it, in all probability you were born with the defect. As stated earlier, these defects affect the uterus, vagina, cervix, and fallopian tubes, and hence, you may find it difficult to conceive and have a healthy and normal pregnancy. To understand what causes these complications, it is important first to have knowledge of normal müllerian tract development in the embryo.
Embryology
When the human embryo develops into a fetus, it forms two tracts side by side. These tracts are known as the Wolffian (mesonephric) and the Müllerian (paramesonephric) tracts. The Wolffian (mesonephric) ducts go on to form the prostate, seminal vesicles, and vas deferens if it is a male embryo. This tract persists in the female embryo, but either remains non-functional or gets wasted due to the lack of testosterone, the male hormone.
At about 8th to 10th week of gestation, the male embryo also secretes an anti- müllerian hormone (AMH), which inhibits the development of the Müllerian (paramesonephric) tract. Just like the female embryo may still have the Wolffian tract as non-functional, the male fetus may still have the müllerian duct in a non-functional state, or it forms into a non-functioning homolog of the uterus.
In a female embryo, there is no production of the AMH. The müllerian ducts develop into the normal female reproductive system, and typically the Wolffian tract dissolves. However, if the Wolffian tract persists long enough to form a kind of a template in the female embryo, complications related to the uterus or kidneys will develop in the female fetus.
In the case of normal development of the female reproductive organs, a portion of the müllerian duct goes on to fuse and form the uterovaginal primordium, a Y-shaped tube. Also known as the UVP, the caudal part of the tube forms the upper portion of the vagina, cervix, and the uterine fundus while the cephalic portion forms the fallopian tubes. When there is a minor or major disruption in this process, uterine anomalies tend to develop. This is typically when the müllerian ducts do not fuse completely (6).
Classification Of Uterine Anomalies
Usually, müllerian duct fusion takes place seamlessly and in a symmetric manner. This may not always be the case always because of environmental and genetic reasons, and it leads to various uterine anomalies. The problem here is that most of these anomalies do not show any signs or symptoms until the woman tries to conceive. This is the reason why there is a lot of debate on classifying them.
While there isn’t a universal classification of müllerian duct abnormalities, the most widely accepted classification is by the American Fertility Society. This classification is as follows (7):
Category 1 – Agenesis And Hypoplasia:
This category of uterine abnormality covers agenesis of the various parts of the uterus, cervix, and fallopian tubes. Most women who experience Category 1 agenesis or extreme hypoplasia may develop severe fertility-related issues but may still have relatively normal hormone cycles. Some women with this agenesis or hypoplasia have a condition called the infantile uterus. This condition also occurs due to a hormonal imbalance called hypopituitarism and is easily treatable as compared to the müllerian duct anomaly related to the infantile uterus.
In hypopituitarism, doctors can treat you with the help of injections of gonadotropins and menotropins, which aid in inducing ovulation and growth of the uterus. But in case the uterus is not developed due to Müllerian anomaly, then the only options for fertility are either uterine transplant or surrogacy. Therefore expert opinion & accurate diagnosis is a must before going for any treatment option.
In complete müllerian agenesis, the vagina does not form properly or is too short. Also, the uterus may be quite small, or it may be completely missing. The condition becomes a concern when the woman goes well past puberty but does not start her menstrual cycles. Women with this rare condition can have children just through surrogacy or uterine transplant. Vaginoplasty may be done in such patients so that they can have a normal sexual experience.
Category 2 – Unicornuate Uterus:
The Category 2 uterine anomaly deals with the uterus unicornis and can be with or without an anlage. If this anomaly is without a rudimentary horn, it is most likely a result of complete degeneration or failure of the Mullerian duct. On the other hand, if a small accessory uterus (called a rudimentary horn) is present, the uterus can support pregnancy until only 20 weeks maximum. After this stage, the uterus tends to rupture. Doctors may recommend a hemi-hysterectomy to prevent this from occurring.
Typically, a unicornuate uterus is rather an uncommon condition, restricted to about 5% of total uterine anomalies. This condition, however, sees the maximum pregnancy wastages. Most women with unicornuate uterus also have a renal defect. A unicornuate uterus is half the size of a normal uterus. The condition is also known as one-horn uterus because of its shape.
Category 3 – Uterus Didelphys:
The Category 3 uterine anomalies occur in about 1 in 2000 women. Again it is a rare condition, and it occurs due to duplication of the müllerian tract. It is prudent to remember that an actual duplication, with two separate vaginas, cervices, and uterine fundus, is a rare condition. Typically, this condition occurs as a top to bottom split of the müllerian duct. Women with this type of uterine abnormality almost always have a kidney abnormality too.
The rarest and also the most problematic, uterine didelphys can lead to miscarriages and breech babies. Because there is a second uterus, there is a higher likelihood of the mother carrying twins if she becomes pregnant with this anomaly. If this happens and the pregnancy is viable, the twins are completely separate, developing individually in different hemi uterus. These twins may be born hours, days or even weeks apart.
Category 4 – Bicornuate Uterus:
The Category 4 uterus bicornis is a more common uterine defect. Like Category 2 and Category 3 anomalies, this uterine abnormality is also a result of the müllerian duct not fusing properly to form a unified uterus. This anomaly is further classified as bicollis – two cervices, or unicollis – one cervix.
While it is a uterine anomaly, the bicornuate uterus does not pose fertility-related issues. Women with this anomaly, however, commonly have breech babies. Also, there is an increased risk of miscarriage in women who conceive with the bicornuate uterus.
Category 5 – Septate Uterus:
The Category 5 uterine anomaly, the septate uterus, is a result of a proper fusion of the müllerian ducts but faulty resorption. The inner partition that separates the two müllerian tracts does not dissolve either partially or wholly. This midline septum lacks protein Bcl-2 that protects the other parts of the uterus. Whether the septum exists partially or entirely, the septate uterus poses maximum pregnancy-related issues, with completely septate uteri showing about 90% pregnancy wastage. Treatment, however, is possible by simple endoscopic lysis of the septum and is highly successful, with almost 100% successful results in the next pregnancy.
Category 6 – Arcuate Uterus:
Known as uterus arcuatus or arcuate uterus, this type of uterine anomaly is typically nothing to be too worried about. In fact, an arcuate uterus is simply a slight variation of a normal uterus. The uterus has a slight heart-shaped appearance, and this happens when the müllerian tracts fail to fuse or have a dysfunctional septum, but to a small degree.
Category 7 – T-Shaped Uterus:
The T-shaped uterus in female infants results from the mother having a medicine called diethylstilbestrol (DES), which was once commonly used to prevent miscarriage. Studies indicate that about 69% of female offspring of women who consumed DES during their pregnancy developed abnormal uterine cavities and have a T-shape with or without dilated cornua. The uterus in these cases tends to be hypoplastic and prone to cervical incompetence. This results in midterm loss of the fetus. These female infants are also susceptible to other histological abnormalities and are more prone to cervical or vaginal cancer at an early age.
Only about 34% of pregnancies with DES uterus go full term, and about 38% of pregnancies end in a miscarriage. Ectopic pregnancies are also common in DES uterus (8).
Symptoms Of Congenital Uterine Anomalies
Congenital uterine anomalies are present at birth, but they rarely exhibit any sign or symptom. Some women may experience pain during their menstrual period, but that is not always indicative of a congenital defect in the uterus. Most of these abnormalities come to the forefront only after recurrent pregnancy loss or infertility problems (7).
How Are Uterine Anomalies Diagnosed?
Most uterine anomalies do not show significant signs or symptoms. It is only when a woman with these abnormalities tries to conceive or suffers pregnancy complications that doctors diagnose them. The following procedures help in the diagnosis of uterine anomalies (9):
1. Vaginal Ultrasound:
A vaginal ultrasound is an internal ultrasound that uses sound waves to capture images of your vagina and other parts of the uterus. To accurately diagnose uterine defects, a vaginal ultrasound is imperative as an abdominal ultrasound over the belly will not clearly indicate the state of your womb.
2. Hysterosalpingogram:
This test requires insertion of a dye into your cervix. After that, the doctor will take an X-ray. It allows the diagnosing physician to evaluate your uterus, cervix, and fallopian tubes. A doctor performs this test only if you are not pregnant.
3. Magnetic Resonance Imaging (MRI):
This test uses magnetic and radio waves to evaluate your uterus. Many healthcare practitioners believe MRI is the most accurate way of identifying a majority of uterine anomalies. MRI has the benefit that it can also be done while you are pregnant as it is safe during pregnancy, unlike CT scans and X-rays.
4. Sonohysterogram:
If a regular ultrasound does not provide clear images of your uterus or the results are inconclusive, the doctor may suggest sonohysterogram. For this test, the sonographer will insert sterile normal saline into your uterus through the cervix. After that, he will use ultrasound to get images of your uterus. Doctors perform this test only on women who are not pregnant.
Treatment For Congenital Uterine Anomalies
The treatment for congenital anomalies may vary depending on the type of anomaly. Among the different types of congenital uterine abnormalities, the septate uterus and any associated vaginal septal defects can be treated with surgery. However, surgical options are usually not recommended for other defects, including bicornuate, unicornuate, and didelphic uterus, since they may cause permanent damage to the uterine muscles (10).
Treatment for congenital uterine anomalies is not always possible. While some treatment options exist, these do not apply to all types of uterine abnormalities. In some cases, the treatment methods can pose further risks. For instance, if the doctor has to surgically remove the septum in the case of a septate uterus, the endometrial lining of the uterus can get affected, which may further have a negative impact on a woman’s fertility.
Hence, if there is a treatment for your uterine anomaly, weigh the risks and advantages before opting for it. Speak to your doctor and also use the Internet to educate yourself to make an informed decision.
Frequently Asked Questions
1. What is the most common uterine abnormality?
According to experts, the septate uterus and bicornuate uterus are the most common congenital uterine anomalies (11). A septate uterus is a normal-shaped uterus with a tissue wall that creates two cavities. On the other hand, the bicornuate uterus is a uterine malformation where half of the uterus is formed (12).
2. Are uterine abnormalities hereditary?
While it may not be alarming to notice specific uterine abnormalities during pregnancy, it can get overwhelming to undergo these changes. However, if you notice symptoms to a more significant extent and feel like it needs immediate attention, you must ensure to pay a visit to your doctor. In such circumstances, you must not skip consulting a healthcare professional as they can explain the situation and prevent you from further complications.
References
- Uterine anomaly.
https://www.columbiadoctors.org/treatments-conditions/uterine-anomaly#:~:text=Congenital%20uterine%20anomalies%20occur%20in - Imaging of Müllerian Duct Anomalies.
https://pubs.rsna.org/doi/full/10.1148/rg.326125515 - Y. Y. Chan, et al; Reproductive outcomes in women with congenital uterine: a systematic review.
https://obgyn.onlinelibrary.wiley.com/doi/10.1002/uog.10056 - L A Ibeto, et al; The risk of preterm birth associated with uterine anomalies, and the clinical utility of serial measurement of cervical length.
https://fn.bmj.com/content/97/Suppl_1/A115.1 - Caron J. Gray and Meaghan M. Shanahan; Breech Presentation.
https://www.ncbi.nlm.nih.gov/books/NBK448063/ - Müllerian Agenesis: Diagnosis, Management, and Treatment.
https://www.acog.org/clinical/clinical-guidance/committee-opinion/articles/2018/01/mullerian-agenesis-diagnosis-management-and-treatment - ASRM mullerian anomalies classification 2025.
https://www.asrm.org/globalassets/asrm/asrm-content/news-and-publications/practice-guidelines/for-non-members/mac2021_manuscript.pdf - T M Chandler, et al; Müllerian duct anomalies: from diagnosis to intervention.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3473390/ - Thomas M. Dykes, et al; Imaging of Congenital Uterine Anomalies: Review and Self Assessment Module.
https://www.ajronline.org/doi/10.2214/AJR.06.0821?mobileUi=0 - Mullerian Anomalies.
https://www.childrenscolorado.org/conditions-and-advice/conditions-and-symptoms/conditions/mullerian-anomalies/ - Uterine Anomaly.
https://www.columbiadoctors.org/treatments-conditions/uterine-anomaly - UTERINE CONDITIONS.
https://www.marchofdimes.org/find-support - MT Connell et al.; Genetic Syndromes and Genes Involved in the Development of the Female Reproductive Tract: A Possible Role for Gene Therapy.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4264624/ - Bicornuate Uterus.
https://my.clevelandclinic.org/health/diseases/22798-bicornuate-uterus
Community Experiences
Join the conversation and become a part of our nurturing community! Share your stories, experiences, and insights to connect with fellow parents.
Read full bio of Dr. Vaishali Sharma
Read full bio of shreeja pillai