
Image: ShutterStock
A subchorionic hematoma is abnormal blood accumulation between the uterine wall and the chorionic membrane. It is one of the many underlying causes that may lead to vaginal bleeding during pregnancy. Vaginal bleeding at any stage in pregnancy needs immediate medical assessment.

Recognizing and monitoring subchorionic hematomas is important because they can affect pregnancy outcomes. Early diagnosis allows for prompt medical intervention, which can help reduce potential risks related to this condition. In this post, we explain the causes, symptoms, diagnosis, side effects, and treatment of subchorionic hematoma.
Key Pointers
- Subchorionic hematoma (SCH) is a rare accumulation of blood between the uterine and chorionic membranes during pregnancy.
- SCH can cause vaginal bleeding during pregnancy and is most common in women who are 10-20 weeks pregnant.
- The exact cause of SCH is unknown, but certain factors such as poor placentation, abnormal implantation of the fertilized egg, age over 35, and blood coagulation disorders may increase the risk of developing SCH.
- Symptoms of SCH include vaginal bleeding, dizziness, abdominal cramping, and pain.
- While some cases of SCH may resolve on their own, others may require medication or hospitalization.
What Is Subchorionic Hematoma?
Subchorionic hematoma (SCH), also termed as subchorionic hemorrhage, is a condition wherein the blood collects/clots between the uterine wall and the chorionic membrane (1). The chorion is the outer membrane between the uterus and placenta, and surrounds the amniotic saciA sac of fluid that holds the fetus in the uterus. . The hematoma leads to placental detachment from the chorion membrane, causing subchorionic bleeding.
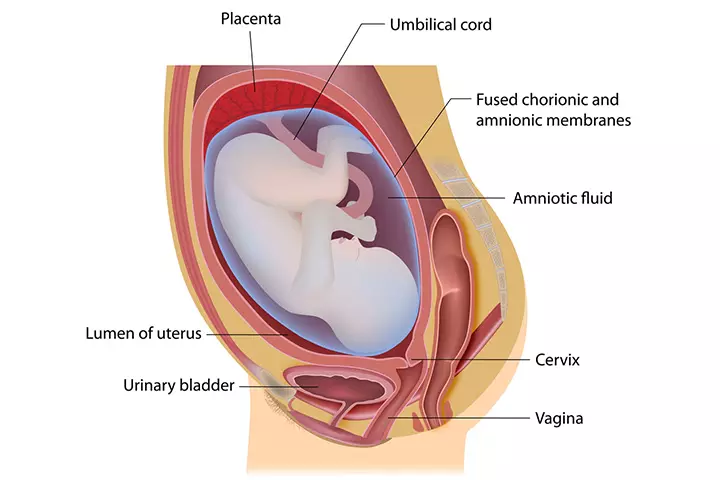
The hematoma leads to placental detachment from the chorion membrane, causing subchorionic bleeding.
How Common Is Subchorionic Hematoma?
The prevalence of subchorionic hematoma is most common in women who are in between 10-20 weeks of gestational age and are experiencing vaginal bleeding. In fact, vaginal bleeding complicates around 16-25% of pregnancies during the first trimester, and nearly 11% of these women who visit a hospital with vaginal bleeding are diagnosed with SCH (2).
Let’s see what leads to SCH and vaginal bleeding.
What Are The Causes Of Subchorionic Hematoma?
The exact cause of SCH is not yet known. It is assumed to be the result of a preexisting autoimmune disease or immunological factors.
Another probable reason is poor placentation, which results in weak vessels that could tear under pressure and lead to low pressure bleeding (3). This condition occurs when the placenta detaches from its plantation site, causing the blood to flow into the chorionic membrane. Thus, a blood clot is formed in the space between the uterus and the placenta (4).
Other factors that may increase the likelihood of developing SCH during pregnancy could be (2)(5):
- Abnormal implantation of the fertilized egg in the uterus
- More in pregnancy conceived via IVF or frozen-thawed embryo transfer
- Multiparous pregnancy
- Uterine trauma
- Blood coagulation disorders (6)
- Scars from previous dilatation and curettageiThe removal of tissue from inside the uterus with a surgical instrument called a curette.
- Mother’s age is more than 35 years (7)
- Uterine malformation
- Pelvic and uterine infections
- History of recurrent pregnancy loss
 Quick fact
Quick factWhat Are the Symptoms Of Subchorionic Hematoma?

One of the most common symptoms of subchorionic hematoma is vaginal bleeding. It can be either in the form of spotting or heavy bleeding. The bleeding may come along with severe abdominal pain or dizziness and cramping.
However, you may not know the reason behind the vaginal bleeding as hematoma can only be detected in an ultrasound scan (5).
Mac Dingle, a YouTuber, experienced vaginal bleeding during pregnancy. Reflecting on the incident, she shares, “I woke up in the morning and noticed more red blood. Although it wasn’t nearly as much as the last time, there was still no cramping or dizziness. However, seeing that color is terrifying at any point, and since there was still no known source for the bleeding, I called my obstetrician’s office.
“They promptly scheduled me for an emergency ultrasound on the same day. During the ultrasound, the technician reassured us that she only saw a beautiful, healthy, bouncing baby. Towards the end, she explained that there was a small subchorionic hematoma, which was most likely the source of the bleeding (i).”
If you experience heavy vaginal bleeding, severe abdominal pain, or dizziness, it’s important to get medical help right away. Seeing a healthcare professional quickly can help keep you and your baby safe.
How Is Subchorionic Hematoma Diagnosed?

The only way to detect subchorionic hematoma is through an ultrasound. Depending on the intensity of vaginal bleeding, the doctor may use abdominal or transvaginal ultrasoundiExamination of the uterus, cervix, ovaries, or pelvic organs by inserting an instrument through the vagina to create sound waves. to determine the reason for the bleeding (8).
An ultrasound can detect the blood clots between the uterus and placenta. The transvaginal method aids in examining the uterine area through the vagina.
Once the scan confirms SCH, the doctor will determine the size of the maternal hemorrhage as the size reflects the intensity of the problem.
Size Of Subchorionic Hematoma
The size of SCH is evaluated (9) depending on the elevation of the chorionic membrane from the uterus wall.
Typically, if the size of the hematoma is 50-66% of the gestational sac then it is large, and less than 20% of the sac is considered small (1). A large hematoma increases the chance of spontaneous abortion, but a small sized one is common during the first trimester (7).
Is Subchorionic Hematoma Harmful?
Smaller hematomas do not harm your pregnancy but result in bleeding. However, larger hematomas carry some serious pregnancy risks such as preterm delivery and placental abruptioniA pregnancy complication in which the placenta detaches from the womb causing deprivation of nutrients and oxygen in the baby. (10). The risks of subchorionic hematoma are:
- Subchorionic hematoma increases the risk of miscarriage in the first 20 weeks of pregnancy. However, vaginal bleeding in an ongoing pregnancy will not increase the chance of a miscarriage (11). Those who experience both bleeding and cramping have a higher risk of threatened miscarriage compared to those without any symptoms.
- SCH, in combination with any underlying pregnancy complication such as stress or injuries, also increases the chances of miscarriage (12).

- The outcome of the pregnancy with subchorionic hematoma depends on the size of the hematoma, gestational age, and the mother’s age (9).
- The other risks associated with SCH include intrauterine fetal growth restriction, pre-eclampsiaiA pregnancy complication characterized by high blood pressure and protein in the urine. , placental abruption, or fetal distress (13).
 Did you know?
Did you know?How Is Subchorionic Hematoma Treated?
Depending on the size of the hematoma, gestational age, and the severity of the symptoms, the doctor would suggest the course of treatment. Here are some common advice and possible treatments your doctor would suggest (5) (7):
- The doctor may order bed rest or advise you to minimize your activities if the hematoma size is small.
- You may need to avoid sexual intercourse during this period.
- The doctor may use estrogeniA sex hormone responsible for the development of female sexual characteristics. or progesteroneiA female reproductive hormone that plays a vital role in menstruation, pregnancy, and breastfeeding. therapy to strengthen your pregnancy. Dydrogesterone is a synthetic progesterone hormone that is administered orally (40mg/day) for treating subchorionic bleeding (14).
- Blood thinners (anticoagulants) (15) may be advised to aid the removal of the blood clot.
- Anti-D immunoglobulin injections would be advised for women who are rhesus negative and are experiencing vaginal bleeding after 12 weeks of pregnancy.
- Your doctor would closely monitor your health for fetal and uterine health.
You may support SCH treatment with some personal care.
In recent years, some other treatment methods have also been evolved to deal with the risk of threatned miscarriage in pregnant women with SCH. Some studies showed the positive therapeutic effects of oral lipoic acid slong with vaginal progesterone for the treatment of SCH. In a few studies, traditional Chinese medicines, including Shoutai Pill combined with progesterone and Bushen Yiqi decoction has also been shown to improve the symptoms of miscarriage and other SCH symptoms (6).
Managing Subchorionic Hematoma
Subchorionic hematoma is a common pregnancy concern which may cause several maternal and fetal complications. While the condition is generally treated depending on the size of SCH and gestational age, certain lifestyle modification can help to manage symptoms and improve pregnancy outcomes. Here are some ways to deal with this pregnancy condition:
- Keep track of any vaginal bleeding during pregnancy.
- You should also look out for an antepartum hemorrhage that is characterized by bleeding from the birth canal after the 24th week of pregnancy (16).
- Avoid heavy work and exercise.
- Stay well hydrated to prevent constipation and straining during bowel movements.
- Take regular small meals with fiber.
- Stay calm and stress-free.
- Don’t miss any appointments with your doctor. Follow the doctor’s guidelines about bed rest and activity levels.

Frequently Asked Questions
1. What is subchorionic hemorrhage ICD 10 code?
Subchorionic hemorrhage ICD 10 code is O45 (17). Since this condition occurs due to the placental abruption, it is put under the category O45 that stands for ‘Premature separation of placenta’.
2. Can you experience subchorionic hemorrhage without bleeding?
Yes. You can have SCH without bleeding because the blood gets reabsorbed in the uterus. Even without vaginal bleeding, the risks associated with SCH remain the same (18).
3. What are the other causes of bleeding during pregnancy?
Some other causes of bleeding during pregnancy are (19):
- Implantation
- Intercourse
- Cervical polypiA small benign tumor in the lower part of the uterus connecting the vagina, the cervix.
- Vaginal infection
- Ectopic pregnancy
- Miscarriage
- Molar pregnancy
4. Can I have a healthy pregnancy with subchorionic hemorrhage?
Subchorionic hematoma is not uncommon in pregnancy, and studies demonstrate that pregnant women who are closely monitored go on to have healthy babies (2).
5. Can subchorionic hemorrhage cause birth defects?
There is a lack of sufficient evidence to support this conjecture. However, a few studies have reported that women with subchorionic hemorrhage are at a higher risk of stillbirth during pregnancy (20).
6. How long does it take for a subchorionic hematoma to go away?
Although there is no fixed time designated for the healing of subchorionic hematoma, a hematoma may shrink on its own or cause complications, depending on the size (5).
Subchorionic hematoma (SCH) during pregnancy is not very common. Nonetheless, it is seen in some pregnant women during the first trimester and is usually caused by auto-immune factors, infections, or other medical reasons. Although vaginal bleeding is a specific indication of SCH, it may not be the only reason, and there could be other causes why you may have spotting or bleeding during pregnancy. Therefore, it is essential to consult a doctor sooner to understand the reasons for vaginal bleeding. In most cases, bleeding due to a small-sized hematoma may not lead to serious pregnancy complications. Nevertheless, your doctor will be the right person to evaluate your condition.
Infographic: How Serious Is A Subchorionic Hematoma?
Subchorionic hematoma may not harm the baby most times. Small-sized hematomas may be resolved without causing any issues. Go through the infographic to learn more about subchorionic hematoma and pregnancy outcomes.
Some thing wrong with infographic shortcode. please verify shortcode syntaxIllustration: Subchorionic Hematoma: What It Is Causes & Pregnancy Risk

Image: Stable Diffusion/MomJunction Design Team
Sometimes pregnant women may experience bleeding during their first trimester. Watch this video to understand why this may happen and what exactly a subchorionic hematoma is.
Personal Experience: Source
MomJunction articles include first-hand experiences to provide you with better insights through real-life narratives. Here are the sources of personal accounts referenced in this article.
i. My Subchorionic Hematoma & Hemorrhage Experience.https://www.youtube.com/watch?v=FEukykN6UNY&feature=youtu.be
References
- Subchorionic hemorrhage
https://radiopaedia.org/articles/subchorionic-hemorrhage-1?lang=us - Christopher P. Bondick et al.; (2025); Subchorionic Hemorrhage.
https://www.ncbi.nlm.nih.gov/books/NBK559017/ - Lim Dee Zhen; (2017); Effects of subchorionic haematoma on pregnancy outcomes.
http://www.amsj.org/archives/6064 - Vaginal bleeding in early pregnancy: patterns predictors and association with miscarriage.
https://cdr.lib.unc.edu/concern/dissertations/bz60cw561 - Subchorionic Hematoma.
https://my.clevelandclinic.org/health/symptoms/23511-subchorionic-hematoma - Tiantian Xu et al.; (2025); Subchorionic hematoma: Research status and pathogenesis (Review).
https://pmc.ncbi.nlm.nih.gov/articles/PMC10865452/ - Subchorionic Haematoma.
https://www.chelwest.nhs.uk/your-visit/patient-leaflets/womens-services/subchorionic-haematoma - A Kurjak et al.; (1996); Subchorionic hematomas in early pregnancy: clinical outcome and blood flow patterns.
https://pubmed.ncbi.nlm.nih.gov/8796766/ - G L Bennett et al.; (1996); Subchorionic hemorrhage in first-trimester pregnancies: prediction of pregnancy outcome with sonography.
https://pubs.rsna.org/doi/abs/10.1148/radiology.200.3.8756935 - Is spotting during pregnancy normal?
https://news.sanfordhealth.org/womens/is-spotting-during-pregnancy-normal/ - Yavuz Emre Şükür et al.; (2014); The effects of subchorionic hematoma on pregnancy outcome in patients with threatened abortion.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4285213/ - Miscarriage – threatened.
https://medlineplus.gov/ency/article/000907.htm - Irina O. Bushtyreva et al.; (2015); Pregnancy Outcomes in Pregnant Women with Subchorionic Hematoma.
https://www.ijbm.org/articles/Article5(3)_OA5.pdf - Dimitrie Pelinescu-Onciul; (2007); Subchorionic hemorrhage treatment with dydrogesterone.
https://pubmed.ncbi.nlm.nih.gov/17943544/ - Blood Clot Treatment.
https://www.stoptheclot.org/about-clots/blood-clot-treatment/ - Antepartum Hemorrhage
https://www.rcog.org.uk/media/pwdi1tef/gtg_63.pdf - ICD-10-CM Index To Diseases And Injuries.
https://ftp.cdc.gov/pub/health_statistics/nchs/publications/ICD10CM/2019/icd10cm_index_2019.pdf - J. Jeong et al.; (2014); The clinical significance of subchorionic hematoma without vaginal bleeding during the first trimester of pregnancy.
https://obgyn.onlinelibrary.wiley.com/doi/pdf/10.1002/uog.13870 - Bleeding During Pregnancy.
https://my.clevelandclinic.org/health/symptoms/22044-bleeding-during-pregnancy - Lim Dee Zhen; (2017); Effects of subchorionic haematoma on pregnancy outcomes.
https://www.amsj.org/archives/6064
Community Experiences
Join the conversation and become a part of our nurturing community! Share your stories, experiences, and insights to connect with fellow parents.
Read full bio of Dr. Monica Agarwal
Read full bio of shreeja pillai
Read full bio of Rebecca Malachi
Read full bio of Reshmi Das
















