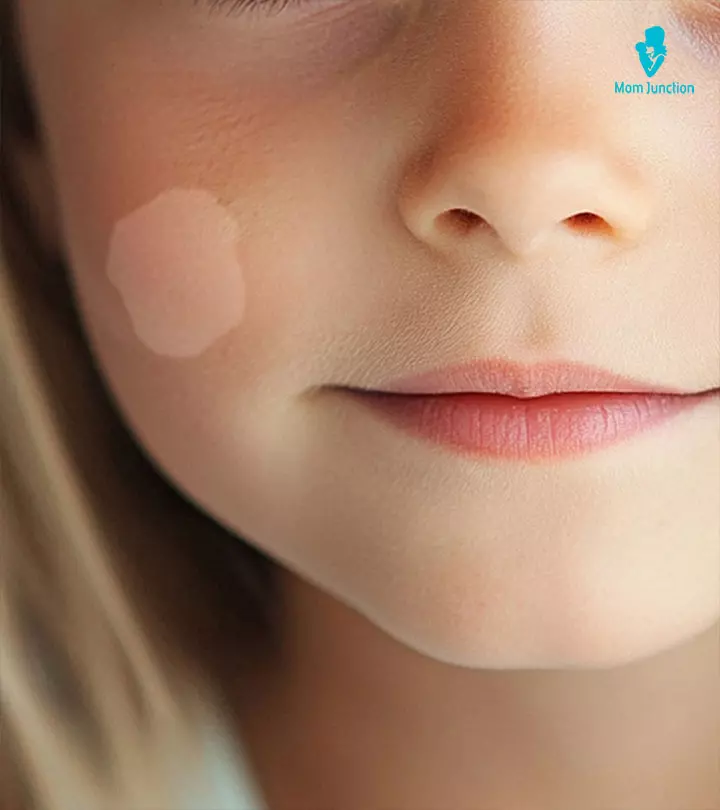
Image: Midjourney/ MomJunction Design Team
Most parents are concerned when they notice white patches on a kid’s face. These white patches or spots are also known as hypopigmented spotsiWhite spots patches on the skin . The discoloration may cause them to be more concerned about any underlying illness than about their child’s appearance. Knowing the common causes may help ease concerns and help you take suitable actions.

Hypopigmented spots on a child’s face can be caused by many different disorders, ranging from self-resolving conditions to diseases that can last a lifetime (1). Therefore, it is advised that you seek professional care for your child for a precise diagnosis and to determine whether there is a viable treatment option.
Read on to know more about the causes, diagnosis, treatment, and prevention of several types of white spots on children’s faces as well as some home remedies.
Key Pointers
- Hypopigmented spots or white patches on a child’s face can occur due to several disorders, ranging from self-limiting conditions to chronic diseases.
- In some cases, white patches can also occur due to vitamin or mineral deficiencies.
- Pediatric evaluation of the spots is essential for early diagnosis of the precise cause and timely initiation of the treatment.
- Over-the-counter (OTC) or commercial lotions and creams purported to cure white spots may not be ineffectual in most cases and may have side effects.
- Always try a home remedy for white patches on the child’s face after thorough guidance from a certified professional.
White Spots On A Child’s Face
Dr. Mykale Elbe, a family nurse practitioner from Mascoutah, Illinois, says, “White patches can be caused by many different things and do not always mean a deficiency. There are viruses, bacteria, and skin conditions that can cause white spots and white bumps on children’s faces for various reasons. It is safe to start with soap and gently clean your child’s face as this can help with some causes. Then, get your child seen by a health professional to determine the cause before adding other solutions, medicated lotions, or supplements.”
There are many reasons for leucoderma dermatosis (skin conditions with white spots) on a child’s face. Sometimes, these leucoderma patches can be due to certain mineral or vitamin deficiencies. You may consult a pediatrician or a certified dermatologist to know the exact cause before attempting treatments with vitamin or mineral supplements.
Over-the-counter or commercial creams or lotions that promise a cure for white spots on the face may not be useful in most cases and may have side effects.
The following skin conditions may cause white spots on a child’s face.
1. Milia
Milia are also called milk spots. These are primarily tiny white bumps rather than patches and usually appear on the face, and you may rarely notice milia on the upper trunk or the limbs. Although milia can be seen at any age, it is common in newborns (2).

- Causes and diagnosis of Milia
Milia is caused by trapping keratin (skin flakes) under the skin surface. You may consult a doctor if milia are not disappearing after a few weeks. The diagnosis of milia is made by visual examination, and no tests are required (3).
- Prevention and treatment of Milia
There is no way to prevent milia, and it often disappears within a few weeks or months. There is no requirement of medical treatments for milia in kids (4).
Home remedies to reduce milia may include (3):
- Wash your kids face daily with mild soap and water
- Pat dry the face after wash
- Do not pinch or scrub milia, since it may cause skin damage and infection
Note: Some parents may confuse baby acne or Epstein pearls with milia. However, acne can cause red bumps and pustules on the face. Epstein pearls are small white-yellow cysts, often look like milia, but these appear on the roof of the mouth and gums (4).
 Quick fact
Quick fact2. Pityriasis alba
Pityriasis alba is a self-limiting, skin condition that causes dry, fine, scaly skin discoloration, and pale marks on the face.
It is common in children and young adults and considered as a type of eczema or dermatitis (5). This condition’s name is derived from the characteristic appearance of the skin. Pityriasis refers to fine scaly appearance and alba for the hypopigmentation or pale skin color.

- Causes of pityriasis alba
Causes of pityriasis alba are not yet discovered. However, atopic dermatitisiA common skin condition that causes itchy, red, and inflamed skin. and dry skin often coexist with it. Sun exposure may make it more visible due to the tanning of the surrounding skin (6).
 Quick fact
Quick factThe purported causes, such as inadequate or excess bathing, low serum copperiIndicates copper deficiency which can cause loss of pigment from the skin , ultraviolet radiation, or Malassezia yeastsiThe group of yeasts which can cause or worsen a variety of skin infections , are not yet proven to cause hypopigmentation (6).
- Symptoms and signs of pityriasis alba
One or more light patches, varying from 0.5 to 5cm in diameter, are a characteristic finding in pityriasis alba (7). Pityriasis alba may cause a slight itch in some children and is not known to cause any other complications.
- Diagnosis of pityriasis alba
This condition can be diagnosed clinically. Physical examination under a wood lampiA special lamp used to identify pigmented or depigmented patches on the skin could diagnose the condition. A skin skin biopsyiSmall amount of skin removed and inspected under a microscope may show mild spongiotic (fluid buildup between cells) dermatitis with melanin deficiency. Scraped skin may also be collected for mycology examinationiTest to detect a fungal disease to exclude the diagnosis of yeast infection (8).
- Treatment for pityriasis alba
Treatment is not recommended for asymptomatic cases. Moisturizing creams are useful for dry skin appearance, and mild hydrocortisone (topical steroid) creams can reduce itch and redness on the spot (8).
Tacrolimus ointment, and pimecrolimus cream, which are calcineurin inhibitorsiMedications that suppress the immune system which help prevent inflammation. , are shown to be effective in some people (7). However, seek expert advice before using any medicines or creams on a kid’s skin. Skin appearance may gradually return to normal within months or two to three years (9).
- Prevention of pityriasis alba
Avoiding sun exposure and using good-quality sunscreen could help reduce the risk of developing the condition (6). Also, avoid using harsh soaps that can dry out and irritate the skin (10).
3. Vitiligo
Vitiligo in children is characterized by depigmented areas on the skin due to the loss of melanocytes. These are the cells that produce the skin pigment called melanin (11).
Vitiligo can affect both sun-exposed and unexposed areas of the body (12). Irregular pigmentation of the lips and graying of hair are often seen in vitiligo (13).
The graph below shows the results of a study conducted on 4523 cases of European ancestry. According to the findings, vitiligo’s prevalence is distributed widely across different age groups. While the mean age of early-onset vitiligo was found to be 10.3 years, the mean age of late-onset vitiligo was 34 years. The study also found that the average age of onset for vitiligo is 25.9 years, with no significant gender-based differences.

The distribution of vitiligo age-of-onset
Source: Early-onset autoimmune vitiligo associated with an enhancer variant haplotype that upregulates class II HLA expression; Nature Communications
- Causes of vitiligo
Exact causes of vitiligo are unknown (11). These pigment irregularities can be due to dysfunction or loss of melanocytes (melanin pigment-producing cells) that give skin color. Genetic factors or an autoimmune condition where the immune system attacks melanocytes could be a reason for it (14). It can affect any race, at any age. However, onset in childhood and teenage years is typical (13).
- Diagnosis of vitiligo
Vitiligo can be diagnosed on physical examination, and the doctor may examine the skin under a wood lamp. Rarely, a skin biopsy is performed, which helps confirm the diagnosis by the absence of melanocytes (pigment cells) on the skin. Thyroid diseases and diabetes are tested since it may increase the risk of vitiligo in many people (15).
- Treatment for vitiligo
Mild vitiligo with fair blemishes may not require treatment, and some spots may disappear over time. There are few treatments that can help improve an uneven skin tone. CorticosteroidiMedication used to reduce inflammation and overactive immune system creams, photochemotherapy (PUVA), narrow-band ultraviolet B therapy (UVB), and depigmentation are a few medical treatments (16). These treatments may have side effects, and, thus, may not be suggested for children since vitiligo spots are harmless. In 2025, the FDA approved a new treatment for vitiligo called ruxolitinib cream (Opzelura™), which can help restore lost skin color. This medication is the only one approved by the FDA for treating vitiligo and can be used in children as young as 12 years old (17).
The following remedies for blotchy skin may help children with vitiligo (18).
- Using sunscreen could reduce the tanning of skin around the vitiligo spots that could highlight the spot.
- Cosmetics such as concealers can help hide the white spots on the skin.
Although vitiligo can be upsetting for many people due to appearance, it is not a medically dangerous condition. Vitiligo is not an infection, skin cancer, or a contagious disease. Children with vitiligo are as normal and healthy as others.
Do not overly bother about covering the vitiligo spots; let your child take it as a part of their skin color. Explain about vitiligo to family, friends, and peer groups to avoid bullying or negative behaviors.
 Be watchful
Be watchful4. Tinea versicolor
Tinea versicolor, also called pityriasis versicolor, is a fungal skin infection that causes a patchy complexion with lighter or darker patches on the skin. Tinea versicolor can occur at any age, but it is most commonly seen in adolescents and young adults (19).

- Causes of tinea versicolor
Tinea versicolor is caused by yeasts that are generally present on the skin. Overgrowth of Malassezia yeasts due to environmental factors, such as warmness and moisture, could result in spotting on skin. Malnutrition and excessive sweating (hyperhidrosis) may also result in overgrowth of yeasts (20).
Note: Pityriasis versicolor cannot be spread from one person to another (not contagious) since most individuals have Malassezia yeasts on the skin (21). This condition is not caused by poor hygiene (22).
- Risks for tinea versicolor
Weak immune systems, oily and moist skin, or hot and humid climatic conditions may increase the risk of tinea versicolor infection. Children on corticosteroid medication may also be susceptible to this condition (23).
- Signs and symptoms of tinea versicolor
Although the white spots may appear on the face, it is common on the chest, back, and upper arms. Patches can be pink or light brown in some people and may have scale-like flakes. Skin change is usually limited to the skin’s outer layer and often does not cause any pain. Mild itching may be present in some cases(24).
- Diagnosis of tinea versicolor
Physical examination is enough to diagnose tinea versicolor in most children. Rarely, doctors may collect skin scraping to confirm the diagnosis (25).
- Treatment for tinea versicolor
Shampoo containing selenium sulfide is the primary method of treatment. If the condition does not resolve, then antifungal or anti-dandruff shampoos can be used. The skin may get better in a short duration in many children. However, it may take several months to get a uniform skin tone. The monthly use of shampoo is recommended to prevent a recurrence (20).
Note: If you do not notice any changes or if there is a recurrence, consult the healthcare provider for more help. They may prescribe oral antifungal medicines or antifungal creams to treat this condition.
 Point to consider
Point to consider5. Idiopathic guttate hypomelanosis
Idiopathic guttate hypomelanosis (IGH) is a skin condition that causes small, white oval spots or fair skin patches. People may often call it white sunspots. IGH is more common in the elderly fair-skinned people than in children and often goes unnoticed (26).

- Causes of IGH
The exact cause of guttate hypomelanosis is not known. Although not yet proven, it is suggested that it may be due to sun exposure (27).
- Diagnosis of IGH
Physical examination is enough to determine the condition causing these discolored spots. Rarely, biopsy samples are taken. There is usually a decrease in the melanocytes in the affected areas, although melanocytes are not completely absent, like in vitiligo (26).
- Treatment for IGH
IGH spots are benign and do not require medical treatment (27). There is no approved cure for this skin condition, and most treatments aim to improve the skin’s cosmetic appearance.
Home remedies may include regular use of sunscreen and physical barriers to prevent sun exposure since it may contribute to hypomelanosis (26).
When To See A Doctor
You may not be able to differentiate between various causes of white spots since they may look alike. Therefore, consult a pediatrician or a pediatric dermatologist if you notice white patches on kid’s face. It is a must to visit a doctor if the white spots spread and are itchy or cause discomfort to the child.
Although most skin conditions do not require specific medical treatments, some causes, such as a yeast infection or vitamin deficiency, can be cured effectively.
Home Remedies For White Spots On The Child’s Face
Maintaining a child’s skin health is essential to their overall well-being. Always try remedies that certified dermatologists recommend for children. Do not bother your child by trying multiple treatments for a chronic condition. White spots caused by nutritional deficiencies can often be managed by ensuring a balanced diet. However, many conditions that cause white spots on the face cannot be cured, and you may only work on ways to cover them, such as using cosmetic products. The use of sunscreen to avoid skin tanning may also help prevent the exacerbated appearance of the white spots.
Frequently Asked Questions
1. Can white patches on skin be cured?
The treatment for white patches or light-colored marks is dependent on the type. Skin conditions such as vitiligo may be treated with treatments such as repigmentation or depigmentation therapy. White patches caused by other skin conditions, such as tinea versicolor and pityriasis alba, might fade with time.
2. Do white patches spread?
If the white patches are due to vitiligo, they may spread over time. The condition might start with a few white patches on the face, and may spread across the body over a few months. While the small patches might switch places, the larger ones may remain intact (28).
3. How to boost the self-confidence of a child with white patches?
White patches in visible regions might affect the self-esteem of a child. Help your child gain their confidence by encouraging them to join support groups. Assist them in conquering their personal goals to help them see that a skin condition does not reflect their personality. Support them constantly, and let them know beauty doesn’t lie in perfection. Help them develop positive thinking habits. Seek professional help if needed.
4. Which vitamin deficiency causes white spots on the skin in children?
Pediatrician Dr. Mubina Agboatwalla says, “White patches on the skin are due to many reasons, one of them being nutritional deficiency. The deficiency of vitamin D, vitamin E, and calcium causes these patches. Therefore, children should include eggs, milk, fruits, vegetables, and vitamin D-containing foods such as cheese and butter in their diet. Moreover, exposure to indirect rays of the sun is essential.”
5. Does eczema cause white patches?
“Eczema is an allergic condition, causing dryness and irritation in the skin. Frequent episodes of eczema can result in slight discoloration of the skin. The pigment may become lighter but the color is not as obvious as white patches,” opines Dr. Agboatwalla.
White patches on a kid’s face may result from various conditions ranging from mild skin lesions to chronic disorders leading to hypopigmentation on the face. Hypopigmented spots due to vitamins and mineral deficiencies may resolve after supplementation or including them in the diet. In contrast, conditions such as vitiligo can leave permanent white patches. Vitiligo spots rarely fade away when the child grows. Lighter spots on the face due to bacterial or fungal infections can be cured with appropriate treatments. If approved by a dermatologist, you may try home remedies since many things may do more harm than good.
Infographic: Hypopigmentation Of The Skin: Other Causes And Management
Often you may notice light or whitish patches on your child’s skin; though they may not always indicate a serious issue, it is ideal to have them evaluated and treated promptly. This infographic details the additional reasons for white patches and how to deal with them to avoid further complications.
Some thing wrong with infographic shortcode. please verify shortcode syntax
References
- Hypopigmentation.
https://my.clevelandclinic.org/health/symptoms/23363-hypopigmentation - Milia.
https://www.pcds.org.uk/clinical-guidance/milia - Milia.
https://raisingchildren.net.au/guides/a-z-health-reference/milia - Milia.
https://medlineplus.gov/ency/article/001367.htm - Pityriasis Alba.
https://www.aocd.org/page/PityriasisAlba - Pityriasis alba.
https://dermnetnz.org/topics/pityriasis-alba - Pityriasis Alba.
https://www.ncbi.nlm.nih.gov/books/NBK431061/ - Pityriasis Alba.
https://www.mottchildren.org/health-library/abp4927 - Pityriasis Alba.
https://www.dermcoll.edu.au/atoz/pityriasis-alba/ - Pityriasis Alba.
https://www.thekids.org.au/contentassets/4f26bf63a4f648c2bedcb9c40ce63074/tki-pityriasis-alba-v2.pdf - Vitiligo.
https://www.niams.nih.gov/health-topics/vitiligo - Vitiligo.
https://familydoctor.org/condition/vitiligo/ - Vitiligo.
https://kidshealth.org/en/parents/vitiligo.html - Overview – Vitiligo.
https://www.nhs.uk/conditions/vitiligo/ - Diagnosing Vitiligo.
https://nyulangone.org/conditions/vitiligo/diagnosis - Vitiligo: Diagnosis and treatment.
https://www.aad.org/public/diseases/a-z/vitiligo-treatment - Vitiligo.
https://www.yalemedicine.org/conditions/vitiligo - Jasleen Kaur Sandhu and Priyanka Sharma; (2025); Skin camouflage therapy.
https://ijdvl.com/skin-camouflage-therapy/ - Tinea versicolor.
https://www.health.harvard.edu/diseases-and-conditions/tinea-versicolor-a-to-z - Pityriasis versicolor.
https://www.nhs.uk/conditions/pityriasis-versicolor/ - Tinea Versicolor.
https://my.clevelandclinic.org/health/diseases/17719-tinea-versicolor - Pityriasis versicolor.
https://www2.hse.ie/conditions/pityriasis-versicolor/ - Tinea Versicolor in Children.
https://www.stanfordchildrens.org/en/topic/default?id=tinea-versicolor-in-children-90-P01932 - Tinea Versicolor (Pityriasis Versicolor).
https://www.cedars-sinai.org/health-library/diseases-and-conditions/t/tinea-versicolor-pityriasis-versicolor.html - Tinea Versicolor.
https://www.hopkinsmedicine.org/health/conditions-and-diseases/tinea-versicolor - Idiopathic Guttate Hypomelanosis.
https://www.ncbi.nlm.nih.gov/books/NBK482182/#:~:text=Idiopathic%20guttate%20hypomelanosis%20(IGH)%20is - Idiopathic guttate hypomelanosis.
https://dermnetnz.org/topics/idiopathic-guttate-hypomelanosis - Vitiligo.
https://my.clevelandclinic.org/health/diseases/12419-vitiligo - Milia.
https://www.ncbi.nlm.nih.gov/books/NBK560481/ - Tinea Versicolor.
https://www.ncbi.nlm.nih.gov/books/NBK482500/
Community Experiences
Join the conversation and become a part of our nurturing community! Share your stories, experiences, and insights to connect with fellow parents.
Read full bio of Dr. Garima Garg Seth
- Dr. Mubina Agboatwalla is the head of the department of pediatrics at Karachi Liaquat Hospital, Pakistan. She has over 20 years of experience in the field of pediatrics and 50 research papers published in international journals including Lancet and JAMA. Dr. Agboatwalla is also a public health specialist specializing in preventive health including nutrition, breastfeeding and infectious diseases, especially diarrhea, polio, and tuberculosis. She has affiliations with the Center of Disease Control Atlanta (CDC), UNICEF, and WHO.
 Dr. Mubina Agboatwalla is the head of the department of pediatrics at Karachi Liaquat Hospital, Pakistan. She has over 20 years of experience in the field of pediatrics and 50 research papers published in international journals including Lancet and JAMA. Dr. Agboatwalla is also a public health specialist specializing in preventive health including nutrition, breastfeeding and infectious diseases, especially diarrhea, polio, and tuberculosis. She has affiliations with the Center of Disease Control Atlanta (CDC), UNICEF, and WHO.
Dr. Mubina Agboatwalla is the head of the department of pediatrics at Karachi Liaquat Hospital, Pakistan. She has over 20 years of experience in the field of pediatrics and 50 research papers published in international journals including Lancet and JAMA. Dr. Agboatwalla is also a public health specialist specializing in preventive health including nutrition, breastfeeding and infectious diseases, especially diarrhea, polio, and tuberculosis. She has affiliations with the Center of Disease Control Atlanta (CDC), UNICEF, and WHO. - Dr. Mykale Elbe is the director of the MSN Nurse Practitioner Program and assistant professor of Nursing at Maryville University. She earned her BS in Nursing and MS in Nursing with a concentration in Family Nurse Practice from Saint Louis University.
 Dr. Mykale Elbe is the director of the MSN Nurse Practitioner Program and assistant professor of Nursing at Maryville University. She earned her BS in Nursing and MS in Nursing with a concentration in Family Nurse Practice from Saint Louis University.
Dr. Mykale Elbe is the director of the MSN Nurse Practitioner Program and assistant professor of Nursing at Maryville University. She earned her BS in Nursing and MS in Nursing with a concentration in Family Nurse Practice from Saint Louis University.
Read full bio of Dr Bisny T. Joseph
Read full bio of Swati Patwal
Read full bio of Anindita Ghatak